May 18, 2018
By some remarkable coincidence, many Mount Sinai Health System buildings have been dedicated or opened in May.
The Beth Israel Hospital opened its first facility in a rented loft in May 1890 and then moved to 196 Broadway the next year. In May of 1892 they moved again, this time to 206 E. Broadway and 195 Division St. Beth Israel remained at this location until the completion of the Jefferson & Cherry Street building in 1902. Beth Israel did not have another May opening until May 15, 1966 when the Linsky Pavilion opened.
Beth Israel’s Jefferson and Cherry Street location

The Linsky Pavilion, which opened in May 1966
On May 17, 1855, a religious service was held to inaugurate the opening of The Jews’ Hospital in the City of New York, which became The Mount Sinai Hospital in 1866. Presiding at the inauguration was Rabbi J.J. Lyons, with Rabbis Leo, Sternberger, Rubin, Cohen, Waterman, Schickler and Tebrich serving as cantors.
The original building of The Mount Sinai Hospital

The second site of the Hospital
When Mount Sinai had outgrown this site, the Trustees decided to move uptown to the block of Lexington Avenue between 66th and 67th Streets. The cornerstone for the new hospital was laid on May 25, 1870 and the completed hospital was opened on May 29, 1872.

The 1904 building along 100th Street
Within 25 years, the Hospital had again filled its site and decided to move to its current home next to Central Park, between 100th and 101st Streets. The Park ensured that the hospital would not again get surrounded by the bustle of the City’s streets. The cornerstone for this new hospital was laid on May 22, 1901. In May 1922, Mount Sinai marked the completion of a massive expansion project that extended the hospital across 100th Street down to 99th Street. This included 1184 5th Avenue, which today is the oldest building on the Mount Sinai campus.
On May 23, 1952, The Mount Sinai Hospital celebrated the dedication of the Klingenstein Pavilion on 5th Avenue.
This was built as Mount Sinai’s Maternity Pavilion, and remains the home of our OB-GYN department. At the same event, the Atran Laboratory and the Henry W. Berg, MD Laboratory buildings were both dedicated as well.

The Klingenstein Pavilion on 5th Avenue

Vice President Ford and Walter Annenberg looking at the portrait of Mrs. Annenberg at the dedication in 1974
And finally, in perhaps Mount Sinai’s biggest dedication, on May 26, 1974, the new Mount Sinai School of Medicine welcomed Vice President Gerald Ford and the Annenberg family to celebrate the formal dedication of the Annenberg Building. When this building opened, it was the thought to be the largest space in this country devoted to medical education.

St. Luke’s Hospital on 5th Avenue
The Mount Sinai Hospital was not alone in its fascination with May for buildings. On May 21, 1857, the St. Luke’s Hospital chapel opened at the Hospital’s first site and a year later (May 13, 1858) the hospital itself opened at 5th Ave between 54th and 55th Streets.
The Woman’s Hospital in the State of New York, which became the Women’s Division of St. Luke’s Hospital in 1952, also had a May dedication tradition. On May 4, 1855 the Woman’s Hospital was opened at 83 Madison Avenue. Almost 50 years later, on May 17, 1904, the cornerstone was laid at a new site at Amsterdam Avenue and 110th Street.

The first home of the Woman’s Hospital

The 1904 west side Woman’s Hospital building
Finally, on May 25, 1965 the Woman’s Hospital opened in a separate building on the St. Luke’s campus on Amsterdam Avenue and 114th Street.

Apr 24, 2018
As the spring very slowly arrives, the tired mind often screams for relief from the challenge of processing complex information. So, here is some Mount Sinai trivia that is guaranteed to interest without straining the brain.
Did you know:
…that in the 17th century there were Native Americans living in East Harlem and there was a stream flowing where the Icahn building now stands?
…that the first year The Mount Sinai Hospital was opened (1855-56), we admitted 216 patients, only five of whom were born in the US, and three of them listed their careers as comedians?
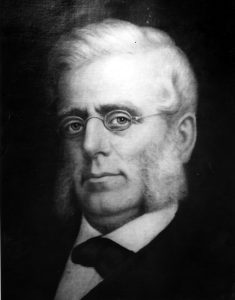
Mount Sinai founder, Benjamin Nathan
…that The Mount Sinai Hospital had a well regarded nursing school that existed from 1881-1971 and that 5 E. 98th Street was the School of Nursing dorm/educational building?
…that when the Hospital moved to its second site at Lexington Ave. and 66th St. in 1872, the Trustees built a large synagogue upstairs and a small operating room in the basement?
…that a Mount Sinai founder, Benjamin Nathan, was murdered in his sleep on a stormy night, and members of his family are still on the Board to this day?
…that Mount Sinai did not have an obstetrical service for the first century of its existence, only offering an OB Service when the Klingenstein Pavilion opened in late 1952?
…that there is a time capsule buried under the directory in the Annenberg Lobby that is scheduled to be opened in 2074, 100 years after it was placed there?
…that Jonas Salk and Henry Heimlich both served their internships at Mount Sinai, Salk graduating in 1942 and Heimlich in 1948?
…that in 1964, Mount Sinai had 1,326 beds, 200 more than we have today?
…that when the first ICU opened at Mount Sinai in 1962, it had five beds and was located in 1184 Fifth Ave., on the 7th floor?
…that in 1993 Mount Sinai School of Medicine became the first in New York State to graduate a class with more women than men?
…that there are at least 43 diseases, syndromes, tests, instruments and phenomena named after Mount Sinai physicians and scientists?
Apr 6, 2018

The photograph above shows the house staff of the Beth Israel Hospital in 1913. By that year, Beth Israel had been active for 24 years, and since 1902 it had been located on Jefferson & Cherry Streets, where this photograph was taken. (The hospital moved to its current location on Stuyvesant Square in 1929.) Although Beth Israel was still a relatively young hospital, it was already a state-of-the-art medical facility, with modern operating rooms, a radiology department, and laboratories for pathology and physiological chemistry. The hospital had a house staff, the precursor of the modern residency system, on which recent medical school graduates would spend two years living at the hospital and acquiring clinical experience.
When the Aufses Archives first acquired this photograph, the identity of the woman standing in the back row was unknown. There were two prints of the photograph in the collection, and they were labeled with conflicting dates, neither of which seemed correct. One print was labeled 1929, but this could not be right, since the clothing appeared wrong for that date and the photograph was clearly taken at the Jefferson Street location. Another was labeled 1908, but in this case, who could the woman have been? The earliest known female doctor associated with Beth Israel was Nettie Shapiro, MD, who served a one-year term as a non-resident extern in 1909, but a comparison with other photographs of Dr. Shapiro showed that it wasn’t her.
The identity of the woman in the photograph remained a mystery until recently, when we discovered a newspaper article in a collection of clippings that provided the answer. The woman in the photograph is Sophie Rabinoff, MD, who was the first female member of the Beth Israel house staff. Born in Russia in 1889, the same year Beth Israel was founded, Dr. Rabinoff came to the United States as a baby with her immigrant parents. She grew up in New York City, where she attended Hunter College before receiving her MD degree from the Women’s Medical College of Philadelphia.

Like other female medical students of her time, in addition to the challenge of mastering the med school curriculum, Dr. Rabinoff had to overcome prejudice against women to continue pursuing a medical career. As the article describes, before taking the competitive examination for the Beth Israel house staff, she had to persuade the hospital management to allow her to sit for the exam. It was only after she came in first out of 31 candidates, ahead of 30 men who also took that year’s examination, that she was admitted. Unlike her predecessor Dr. Shapiro, who as an extern did not live in the hospital or serve the full two-year term, Dr. Rabinoff became a full member of the house staff, with all the accompanying responsibilities and privileges. Unfortunately, 1913 is one of the few years for which the Aufses Archives does not have the minutes of Beth Israel’s trustees or medical board, so we have no record of the debates that might have accompanied her admission.
The photograph in the newspaper article was clearly the same person as the woman in the photograph, confirming that this was an image of Dr. Rabinoff and the rest of the 1913 house staff. A search for additional information on Dr. Rabinoff revealed that she went on to a distinguished career in public health, as documented by her entry in the Jewish Women’s Archive Encyclopedia. After her time at Beth Israel, Dr. Rabinoff served with a Hadassah medical mission in Palestine before returning to New York and becoming a public health officer. She worked for two decades for the Department of Health, where she was responsible for overseeing public health programs in various parts of Manhattan and the Bronx, before joining the faculty of the New York Medical College in 1939. At her passing in 1957, she had recently retired as Director of the College’s Department of Public Health and Industrial Medicine.
Mar 23, 2018
 A new finding aid for The Col. Henry H. M. Lyle Collection of World War I Photographs and Documents, 1916-1943, was recently published and made available to researchers on-line (http://icahn.mssm.edu/about/ait/archives/collection/henry-lyle). The collection includes 200 photographs from World War I, maps and documents used during the war, some correspondence, and reprints of articles by Lyle.
A new finding aid for The Col. Henry H. M. Lyle Collection of World War I Photographs and Documents, 1916-1943, was recently published and made available to researchers on-line (http://icahn.mssm.edu/about/ait/archives/collection/henry-lyle). The collection includes 200 photographs from World War I, maps and documents used during the war, some correspondence, and reprints of articles by Lyle.
The heart of the collection is the photographs taken in France during World War I, which depict often dramatic or surprising images of the war. There are views of hospital stations, barracks, and outdoor equipment (some include large defensive weapons), transportation of wounded soldiers, field dressing stations, supply trains, and troops on the battlefields. Interior views document soldiers, patients, operating rooms and special treatment rooms. A number of the images display the effects of mustard gas and other brutal wounds sustained by soldiers, while others capture the unit compound against the French countryside in an oddly artistic fashion. Still others provide a view of everyday life in the compound – washing clothes, unloading shipments of supplies and such, but which brings to life the challenges of a large group of people living in one spot at that point in time. Laundry meant picking lice off of clothes; unloading supplies meant huge piles of boxes; transporting wounded soldiers sometimes meant walking through ankle-deep mud. The collection also captures images of foreign soldiers in national uniforms, some riding horseback, a lifestyle that is very different from the standard U.S. soldier’s, which adds an interesting, and occasionally humorous, side to the war.
Henry Hamilton Moore Lyle, MD, was a noted surgeon and decorated soldier. He was born in Northern Ireland in 1874. His family immigrated to Ontario, Canada when Lyle was a boy. He graduated Cornell in 1896, and went on to Columbia University’s College of Physicians and Surgeons, graduating in 1900. He took an internship at St. Mary’s Hospital for Children and at New York Hospital and a year’s surgical internship at St. Luke’s Hospital (1901-1902) before joining St. Luke’s surgical staff in 1904 and where he remained on staff until his death.
It appears that Lyle spent the year between his internship and surgical appointment traveling abroad, visiting clinics in Great Britain, France and the German-speaking countries. This familiarity with Europe may have led to his voluntary enlistment in World War I two years before the U.S. was formally involved in the conflict. In 1915 he took leave from his private practice and hospital positions in New York and spent six months as Chief Medical Officer of American Ambulance Hospital B, Juilly, France.
In 1916 he again took a leave and returned to France to serve for several months as Chief Surgeon of Ambulance d’Annel (Longueil, France). In April 1917 when the US entered the conflict, he joined the U.S. Army Reserve and in May was ordered to active service. In June he organized the United States Army Evacuation Hospital No. 2 at Camp Benjamin Harrison, and was appointed its commander when it left for France in January 1918.
In September 1918, Lyle was made Director of Ambulances and Evacuation of the Wounded for the First Army. During the ensuing Meuse-Argonne offensive, over 125,000 sick and wounded were brought to the railhead hospitals under his supervision. In recognition of his outstanding service, particularly during the Meuse-Argonne offensive, where the Evacuation Hospital No. 2 played a major role as one of two front line hospitals established in the Zone of Combat, he was decorated with the Distinguished Service Medal (U.S.). Lyle was also awarded the British War Medal and the British Victory Medal.
When the war ended Lyle returned to New York and medical practice at St. Luke’s Hospital, where his reputation as an outstanding surgeon followed his successes in battle. Lyle retired from medical practice in 1938, though remained a Consulting Surgeon at St. Luke’s until his death from coronary thrombosis on March 11, 1947.
Feb 21, 2018
Soon the Match will be upon the fourth year class and after months of deciding on a field, debating on various institutions, filling out paperwork and then smiling bravely through interviews, the new doctors will be on the resident staff of a hospital. This complex system of ‘matchmaking’ began in 1952 and replaced the practice of individuals applying to various residency programs, perhaps being measured against changeable and very subjective criteria.
In the early years of the 20th century, The Mount Sinai Hospital had in place a rigorous testing program to help winnow the number of applicants, leaving the ‘best and the brightest’ to face additional testing. Each year several hundred medical students would sit for the examinations that would lead to the selection of the twelve newest members of the house staff. The first day’s written examination was number coded, with the individuals’ names hidden so favoritism could not occur. The next day, the top scores were posted, and the 60 highest scorers would return for oral exams given by the medical staff. The questions were broad and usually designed to show a wide knowledge in the basic sciences and clinical medicine, as well as critical thinking skills. Questions on art or literature were not unknown, depending on the faculty member’s interests. The exam evolved over time to be more rigorous, and eventually recommendations from medical schools deans were also sought.
In 1930, these were some of the written questions the applicants were posed. How would you do?
1. In what stages of the following diseases would you terminate early pregnancy? a. Tuberculosis of the lungs b. Nephritisc. Diabetes d. Valvular heart disease
2. Under what conditions would you select for anesthesia? a. Chloroform b. Ether c. Nitrous oxide d. Spinal e. Local f. What special contra-indication for each?
3. In what illnesses may the joints be involved?
4. In what extra abdominal conditions may abdominal symptoms appear?
5. A patient has been operated upon for an acute gangrenous appendicitis with abscess. He had one chill prior to operation. Post-operative course is marked by fever of 102 to 104; high leucocytosis; polynucleosis. X-ray examination of the chest and right hypochondrium shows moderate elevation of right diaphragm. Discuss possible causes of the high temperature.