How did Mount Sinai become a global leader in cardiovascular care and research?
While we can cite many firsts, such as the first use of an electrocardiograph machine in the United States at The Mount Sinai Hospital in 1909, generations of our pioneering health care professionals have played pivotal roles in advancing our knowledge of cardiovascular disease, leading to the development of life-saving interventions and treatments.
In October 2023, Mount Sinai Heart was renamed Mount Sinai Fuster Heart Hospital, in honor of Valentin Fuster, MD, PhD, who is its President and the Physician-in-Chief of The Mount Sinai Hospital. Dr. Fuster has led our progress in cardiology for 41 years, and his commitment to education, research, and discovery has influenced cardiovascular care worldwide. In recognition, The Arthur H. Aufses, Jr., MD Archives staff researched and assembled an exhibit in the Annenberg lobby (on view from December 2023 to May 2024) showcasing some of Mount Sinai’s historic contributions that revolutionized the way we understand and treat heart conditions. The below all pertain to the Mount Sinai Hospital, but the original exhibit included history from the collections of St. Luke’s and Roosevelt Hospital (now Mount Sinai Morningside and West) and Beth Israel Hospital (now Mount Sinai Beth Israel).
1909
First electrocardiograph machine acquired for use at Mount Sinai Hospital by Alfred Cohn, a pupil of Sir Thomas Lewis. This is cited as the first use of an EKG machine in United States. Specialty of cardiology begins to develop at MSH, and by 1927, 13,000 EKGs had been performed here.
1915
The Mount Sinai Hospital established one of the first electrocardiography departments in the country under the direction of Dr. Bernard S. Oppenheimer. Doctors previously had only learned the techniques while training in Europe. The hospital’s wards were wired for connection to EKG. In 1917, Dr. Oppenheimer was awarded an American Medical Association gold medal for an exhibit on electrocardiographic changes associated with myocardial infarction (heart attack).
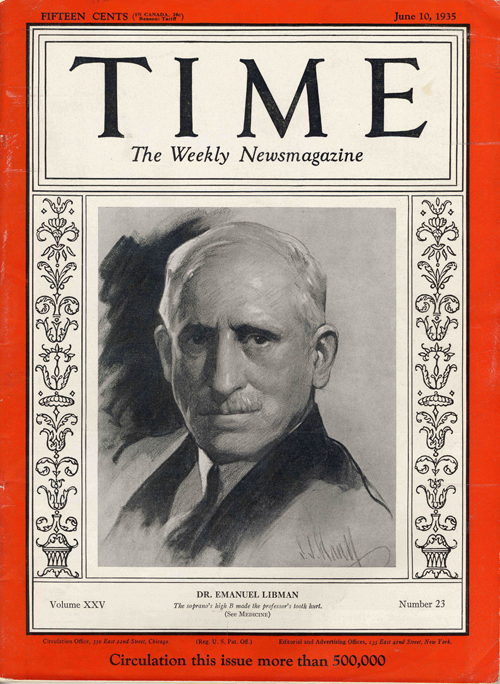
One of Mount Sinai’s giants was Dr. Emanuel Libman. His skills as an internist were renowned— Albert Einstein said he had ‘‘secret-divining eyes.’’ Dr. Libman started as an intern at Mount Sinai Hospital from 1894-1896 and then studied bacteriology and pathology in renowned clinics in Berlin, Vienna, and Munich. In 1897, he published his description of Streptococcus enteritis (later named Streptococcus Libman), which causes focal infection of the intestine. In 1904, Libman, using a gift from Trustee Adolf Lewisohn to build a laboratory building at Mount Sinai Hospital, established a separate department of bacteriology and serology. He went on to study meningococci, streptococci, and Bacillus pyocyaneus, known today as pseudomonas aeruginosa, and became an outstanding bacteriologist. His use of blood cultures to diagnose disease was another major contribution. His seminal work, published in 1910, dealt with the pathogenesis of subacute bacterial endocarditis, which he elucidated through bacteriologic, pathologic, and clinical studies. He introduced the terms “acute” and “subacute” and called attention to the color of the skin and many other clinical features of bacterial endocarditis. In 1924, along with his student, Dr. Benjamin Sacks, Libman first described Libman-Sacks endocarditis (LSE). Widely venerated for his teaching and introduction of clinical conferences in 1905 (known today at Grand Rounds), he worked at Mount Sinai from 1898 until his death in 1946.1
So numerous, original, comprehensive and important have been the studies of the heart emanating from the wards and laboratories of Mount Sinai Hospital that I think one can correctly speak of the Mount Sinai school of cardiologists, of which [Emanuel] Libman was the founder and guiding spirit
– William H. Welch, MD (1850-1934), one of the four founders of Johns Hopkins
1929
Dr. Arthur M. Master devised the prototype for today’s cardiac stress test, the “Master Two-Step”. This was the first exercise test to be standardized for the weight, height, and sex of the patient and evaluated the function of the heart through blood pressure and pulse rate measurements taken before and after exercise. Along with the work of Dr. Simon Dack, this ended an era when total bed rest was prescribed for cardiac cases, noting that lowered caloric intake and moderate exercise are beneficial, while total rest is harmful.
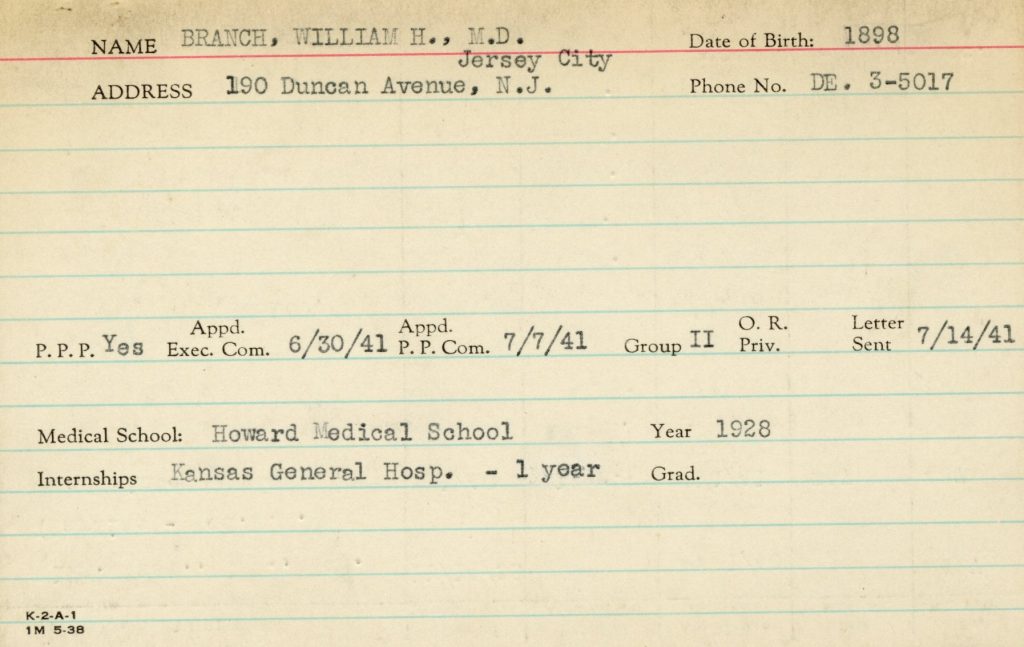
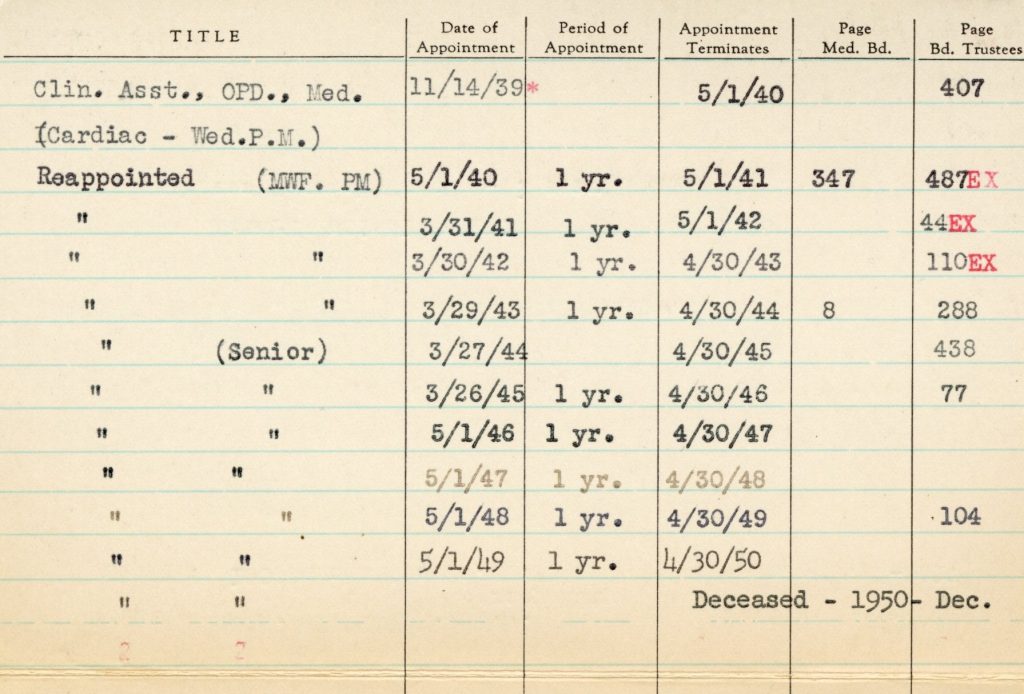
In 1934 Dr. W. Harold Branch joined the Mount Sinai Hospital as a volunteer physician. Dr. Branch was a research member of the special cardiac clinic from 1934 to 1950, where he eventually became Senior Clinical Assistant. From New Jersey, he attended Lincoln University (1920), Howard University Medical School (1928), New York University, Columbia University, and Dr. Branch observed and documented acute coronary occlusion in African Americans, which challenged existing theory on that subject. In 1937, he published an article about a case of sudden simultaneous bilateral embolism of the popliteal arteries, which in 2022 was still considered a ‘rare diagnosis.’ On being elected to membership in the American Heart Association, the New York Times quoted him, saying he “believed he is the only Negro member of the group,” making him the first Black man to be a member.2 He worked at many hospitals in the metro area until his death of a heart attack while riding the bus in 1950.3
1947
Cardiovascular Research Group formed as an interdepartmental entity under the direction of Dr. Marcy Sussman. Some of the earliest studies of angiography and congenital heart disease are performed. The group included the Hospital’s cardiographers and its other experts in various aspects of the physiology and pathology of the heart. Out of their work came two new developments. The first, on the scientific side, was a detailed study of the lesions in congenital heart disease, for which several new techniques and instruments were devised. The second grew out of the realization of the practical advantages of the pooled knowledge of the group as a unit, as well as their special equipment and their skill in using it. Other members of the Medical Staff, confronted by the extremely difficult technical problems involved in diagnosis and treatment of patients with cardiovascular disease, either as the main problem or as a complication in other illnesses, began referring such patients to the group. Also in 1947, the cardiac catheterization laboratory was established.
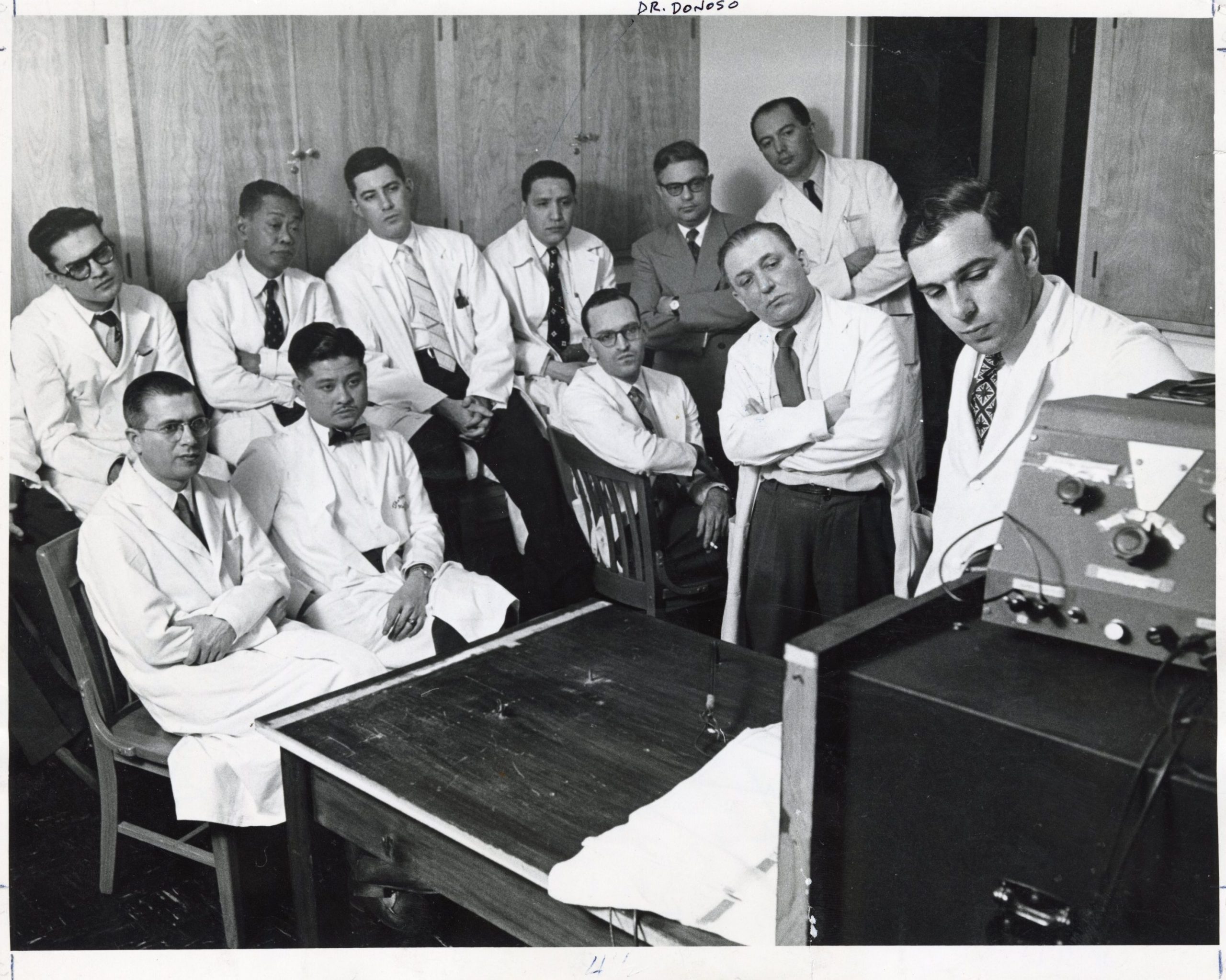
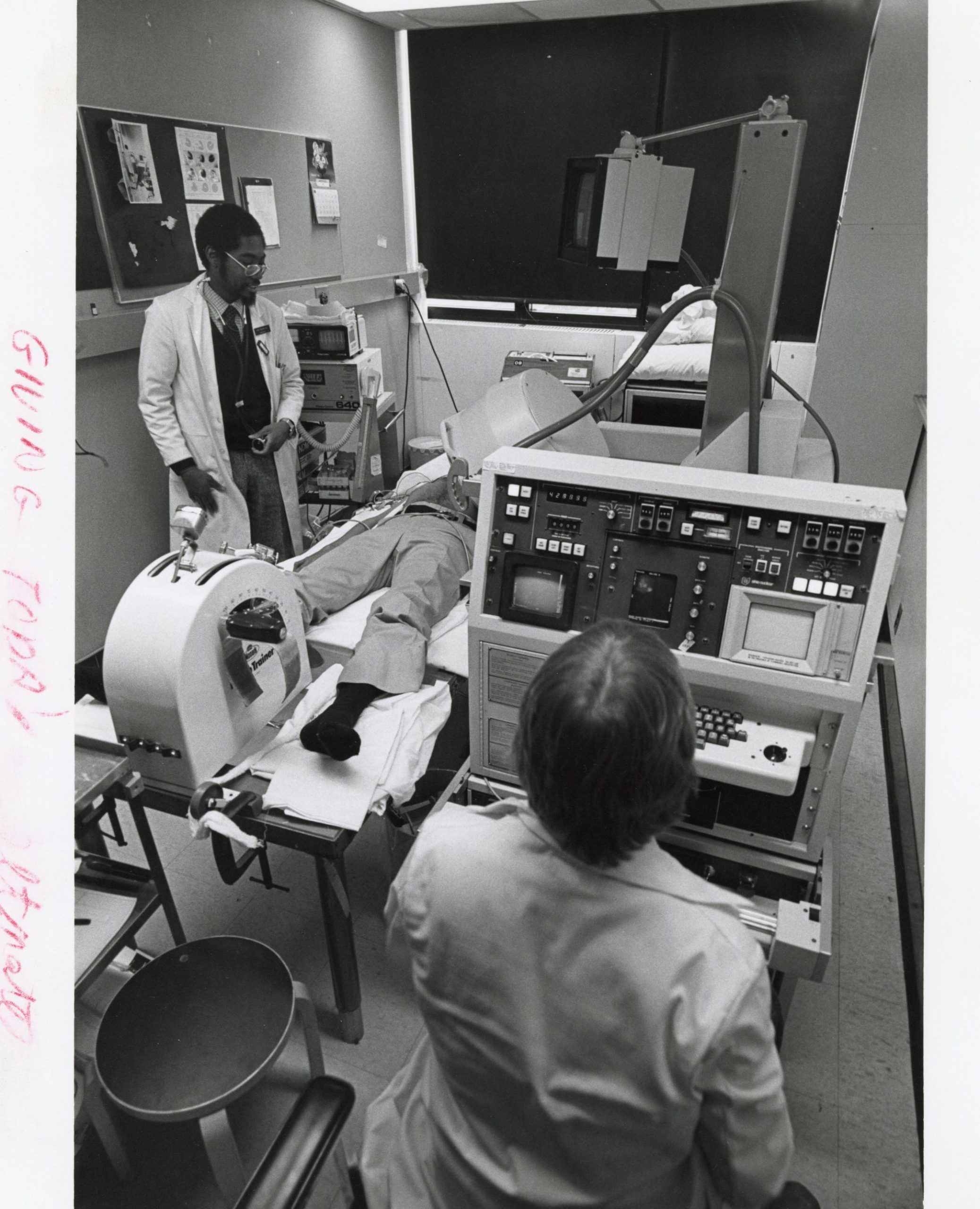
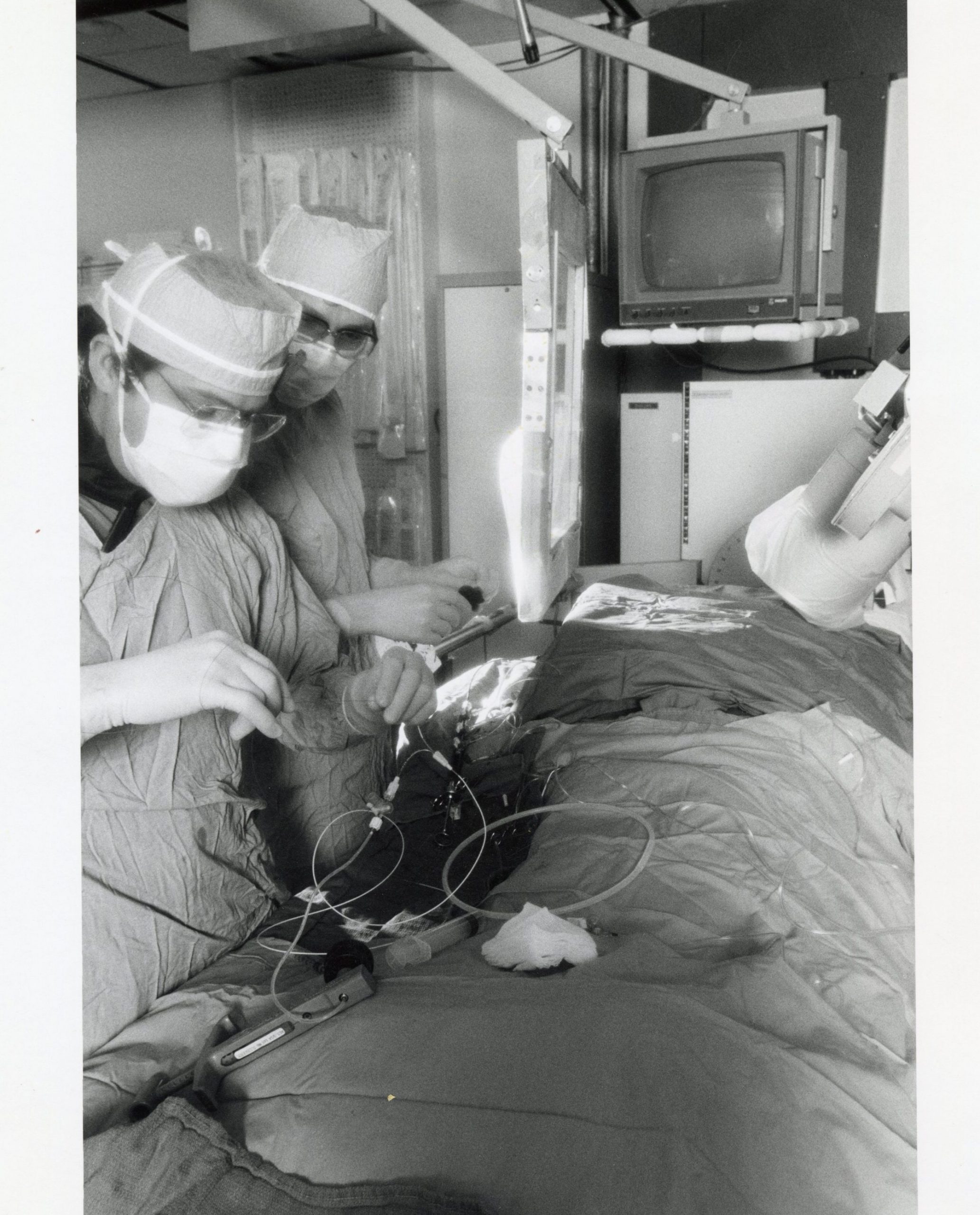
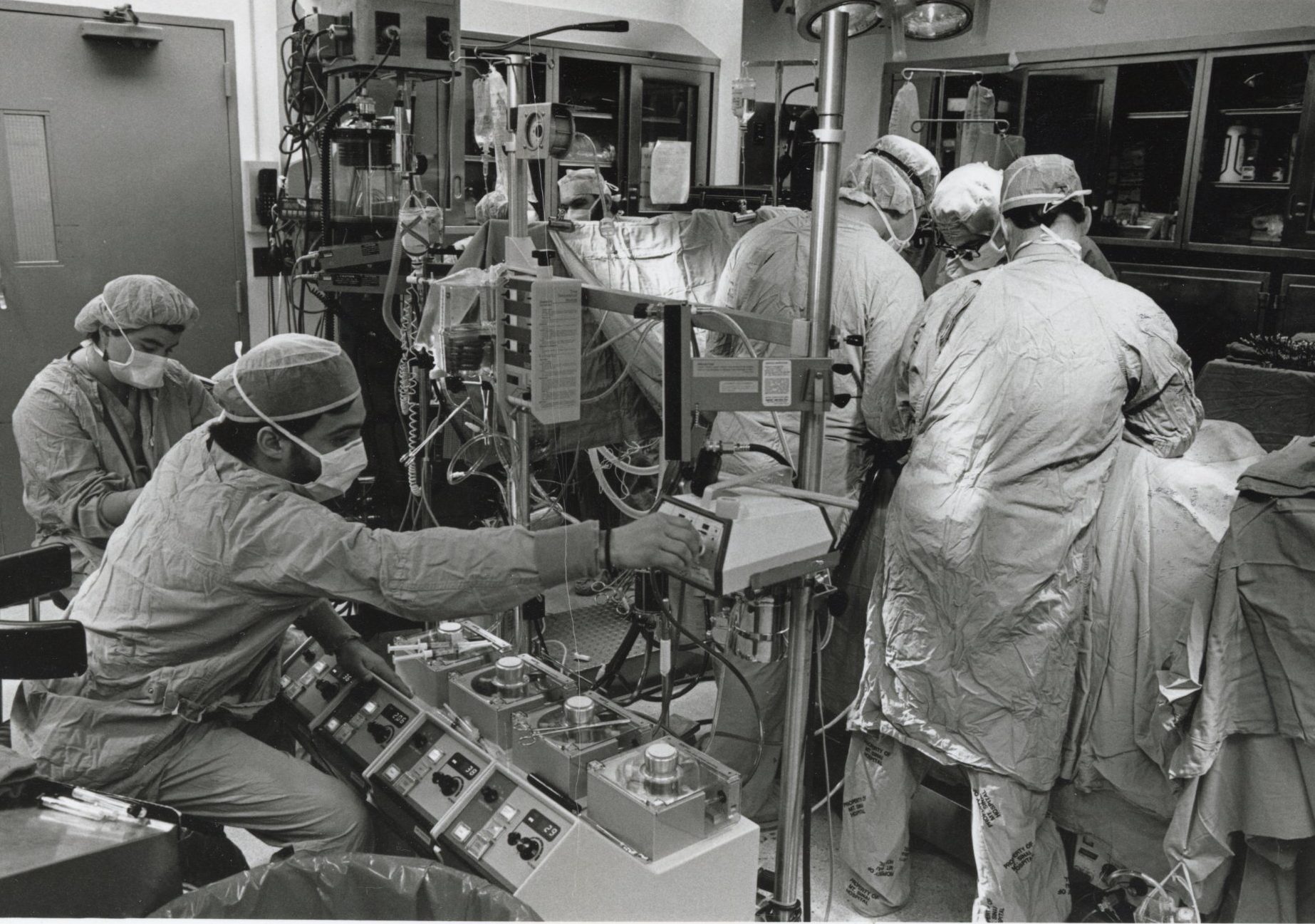
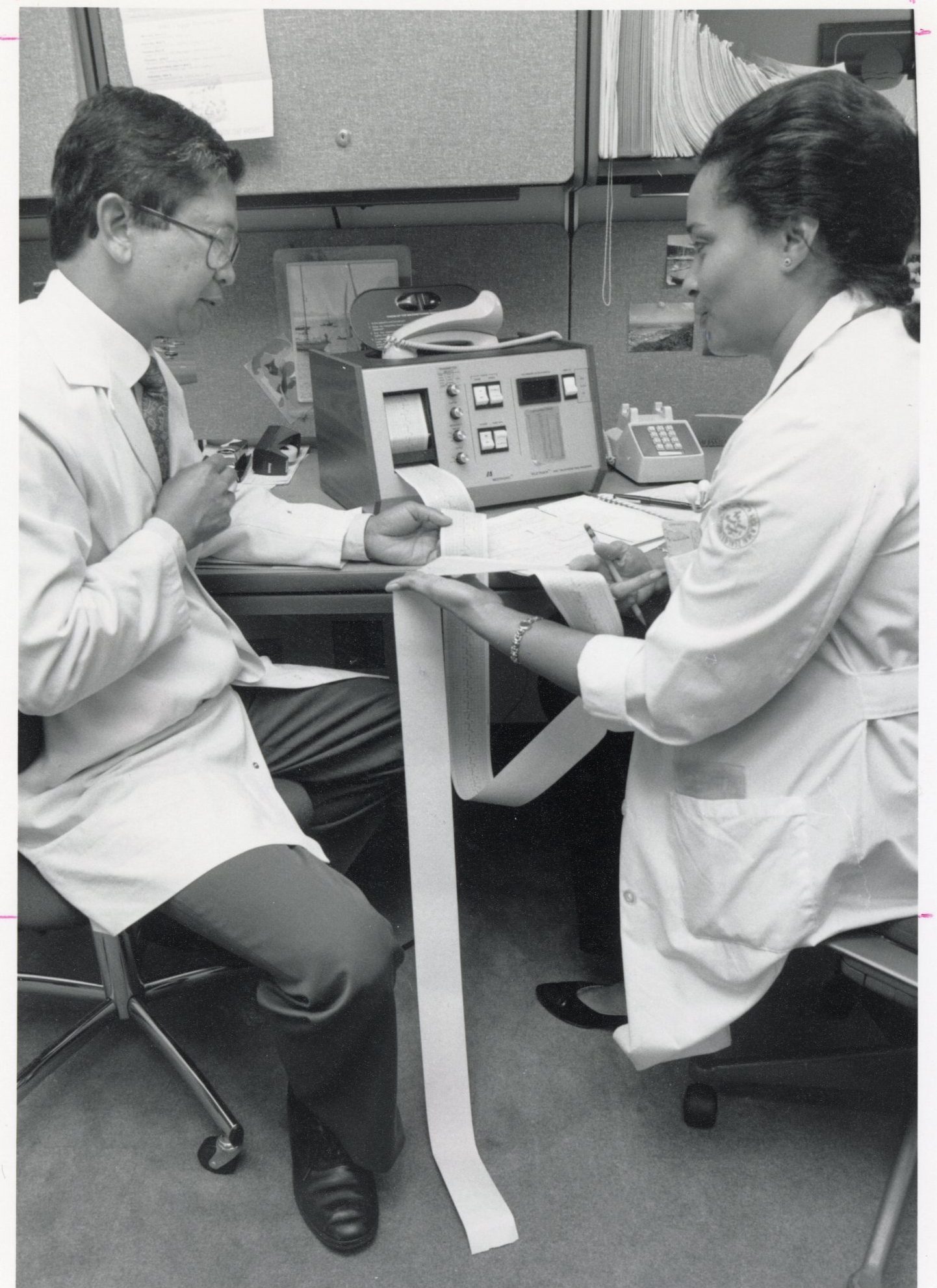
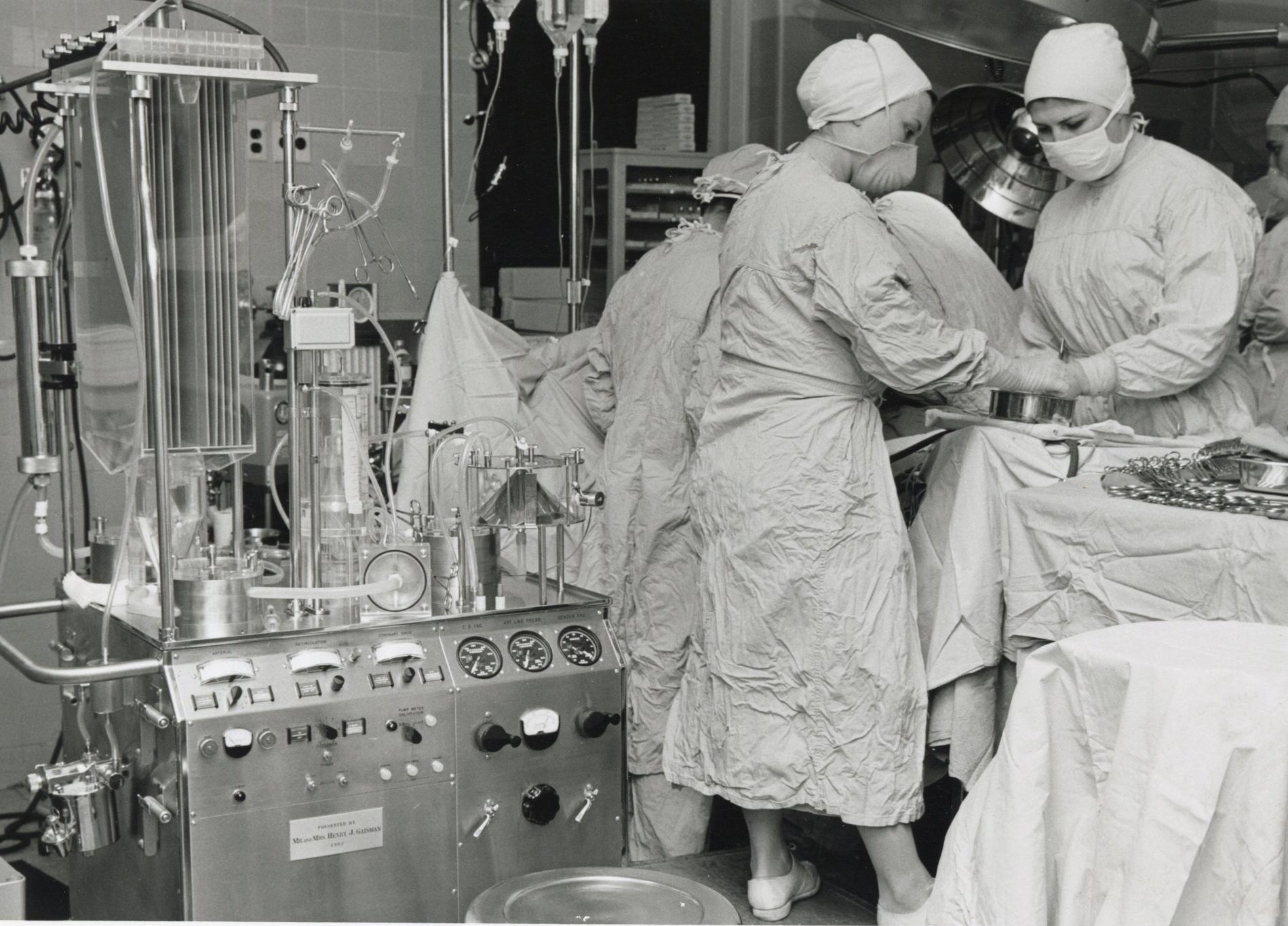
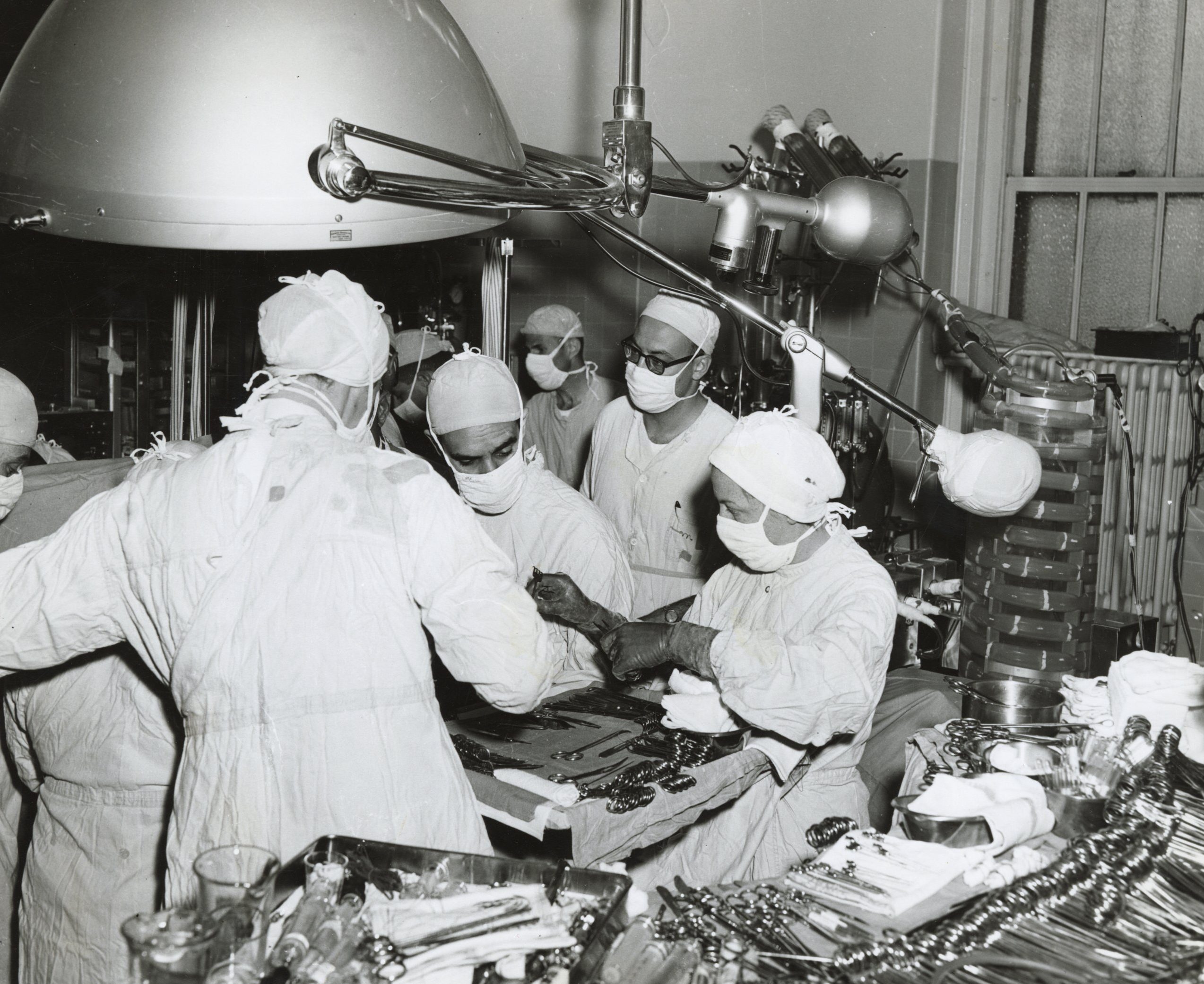
While these machines may look bulky and outdated, they were the cutting-edge technology in their day. Keeping pace with the latest and most efficient equipment remains critical to providing the best patient care. Used in the early days of pioneering cardiac treatments, these were used to perform angioplasties, open heart surgery, radionuclide stress tests, pacemaker interpretation, among others. This group of pictures span from the 1950s to the 2000s.
All images are from the Photograph collection on The Mount Sinai Hospital and Icahn School of Medicine at Mount Sinai
1956
Cardiology was established as a division within the Department of Medicine. Dr. Charles K. Friedberg was appointed Chief.

Also in 1956, a separate residency was established for Cardiology–Nanette Kass Wenger, MD was appointed the first resident, hence also Chief Resident. She was among the first physicians to focus on coronary heart disease in women and to evaluate the different risk factors and features of the condition across genders. In 1958, she moved to Atlanta to become a senior resident in medicine at Emory University. Dr. Wenger conducted her clinical practice at Grady Memorial Hospital and was named director of cardiac clinics and director of the ambulatory electrocardiography laboratory in the 1960s. In 1971 she was appointed full professor of medicine, and in 1998 she became the chief of cardiology. Dr. Wenger has authored and co-authored more than 1,600 scientific and review articles and book chapters. Dedicated to her professional organizations, she was also a founder of the Society of Geriatric Cardiology. She received numerous awards, and in 2004 Dr. Wenger received the Gold Heart Award, the highest award of the American Heart Association, and as well as the Lifetime Achievement Award from the American College of Cardiology.
1958
Mount Sinai Hospital’s Simon Dack, MD, became the first editor-in-chief of the American Journal of Cardiology and developed it over 25 years into one of the world’s most prestigious medical journals. In 1988, the journal became the official Journal of the American College of Cardiology, with Dr. Dack remaining as editor-in-chief.
1950s-1970s Research
Considerable research was performed in the Division of Cardiology. This included projects in: heart failure by Richard Lasser, MD; cardiogenic shock by Leslie Kuhn, MD; computerized ECGs by Leon Pordy, MD; heart block by William Stein, MD; vectorcardiography by Arthur Grishman, MD; hemodynamics by Howard Moscovitz, MD and Alvin Gordon, MD; and echocardiography laboratory work by Louis E. Teichholz, MD. Additionally, Ephraim Donoso, MD was cited as an outstanding clinical teacher.
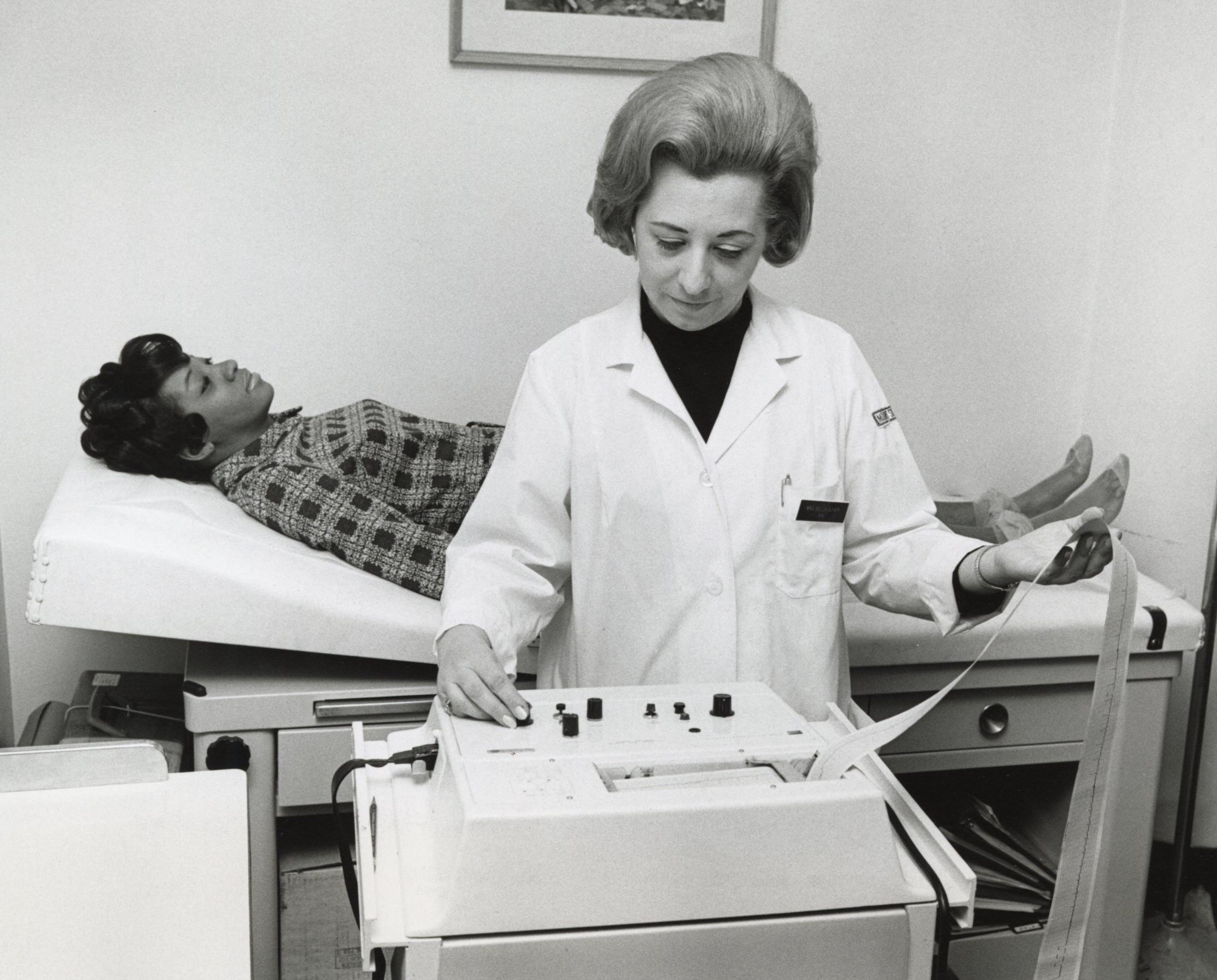
“Mrs. Bel Scher, supervisor of cardiology at Mount Sinai Hospital, has worked at her profession for fifteen years. She trained at one hospital, then worked at several others, even setting up a department of neurology at one of them. Posing as the patient is Miss Dorothy Rucker, who is a technician in the ECG department. In 1967 the average age of the 28 million working women in the U.S. was 41 years.”
1969: Drs. Pordy and Chesky, go over a visitor’s cardiogram they have just taken, while Teodorina Bello, technician, makes a log entry. After running 172 EKG tests on physicians who visited the Mount Sinai booth, Dr. Pordy comes to the conclusion that many doctors should see a doctor.

1983
Valentín Fuster, MD, PhD was recruited from the Mayo Clinic to serve as the Chief of Cardiology. Dr. Fuster was already well known for his research on the relationship between platelet function and atherosclerosis, which helped unify researchers in these areas.
All of the information presented here was sourced from The Arthur H. Aufses, Jr., MD Archives.
Learn more about Mount Sinai’s cardiology work today, at this link.
Post authored by J.E. Molly Seegers, MS, MSLIS. Exhibit contributions by staff archivists Stefana Breitwieser, MLIS and Michala Biondi, MA.
- 1.Archival description containing references to Emanuel Libman. The Arthur H. Aufses Jr., MD, Archives. https://archives.mssm.edu/informationobject/browse?topLod=0&names=1042
- 2.Negro Physician Honored. The New York Times. January 28, 1936:11.
- 3.Harold W. Branch, Cardiac Specialist. The New York Times. December 5, 1950:32.