May 28, 2020
Mount Sinai physicians have a long tradition of making important contributions to the scientific literature. A good example is the following case from the 1910s, when typhus swept the world, killing thousands of people.
In 1910, Nathan Brill, MD, a doctor in the Department of Medicine, published a description of what he thought was the endemic form of typhus; this became known as Brill’s Disease. (Later Hans Zinsser showed that it was not endemic, but a mild recrudescent form of epidemic typhus and the name was changed to Brill-Zinsser disease.) In 1913, Harry Plotz, MD, an intern working in Mount Sinai‘s Pathology Laboratory, believed that he had discovered an organism that caused typhus. He published a Letter in JAMA in 1914 outlining his research.

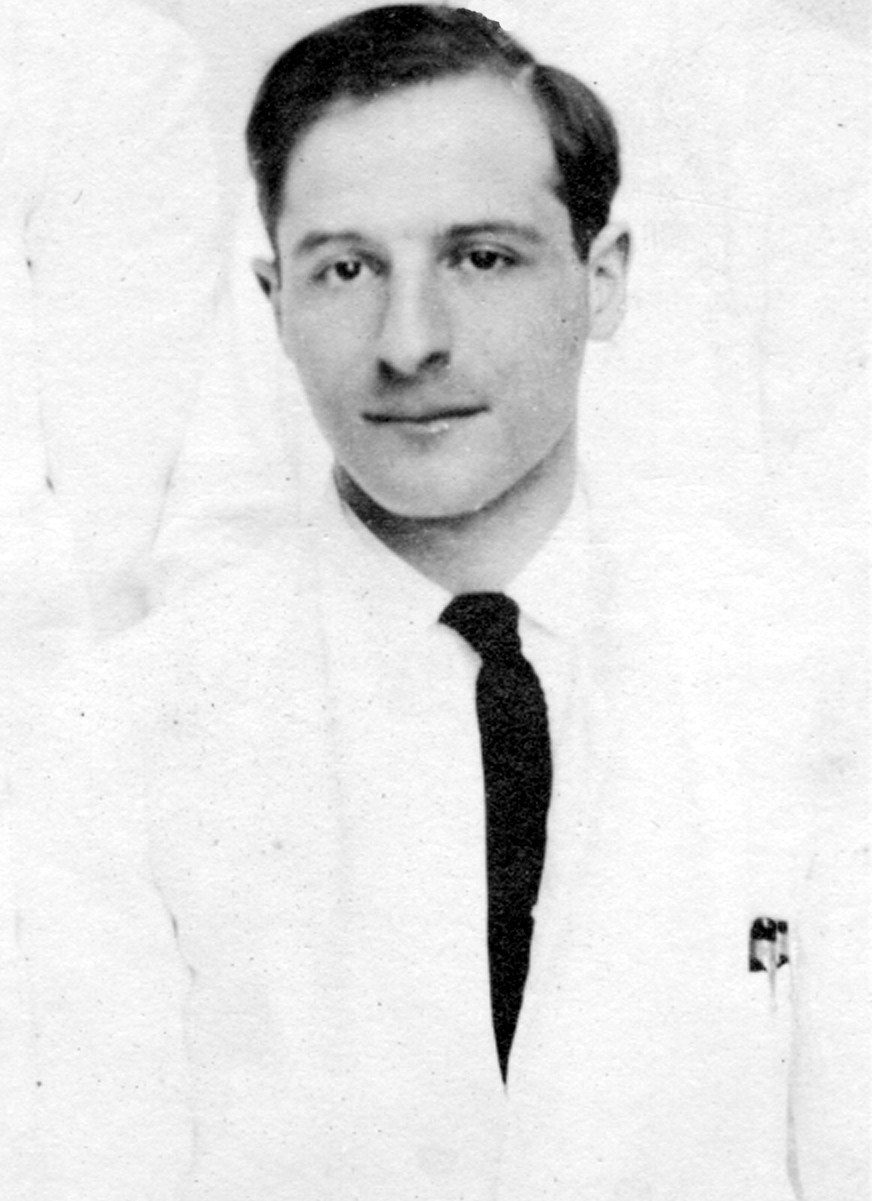
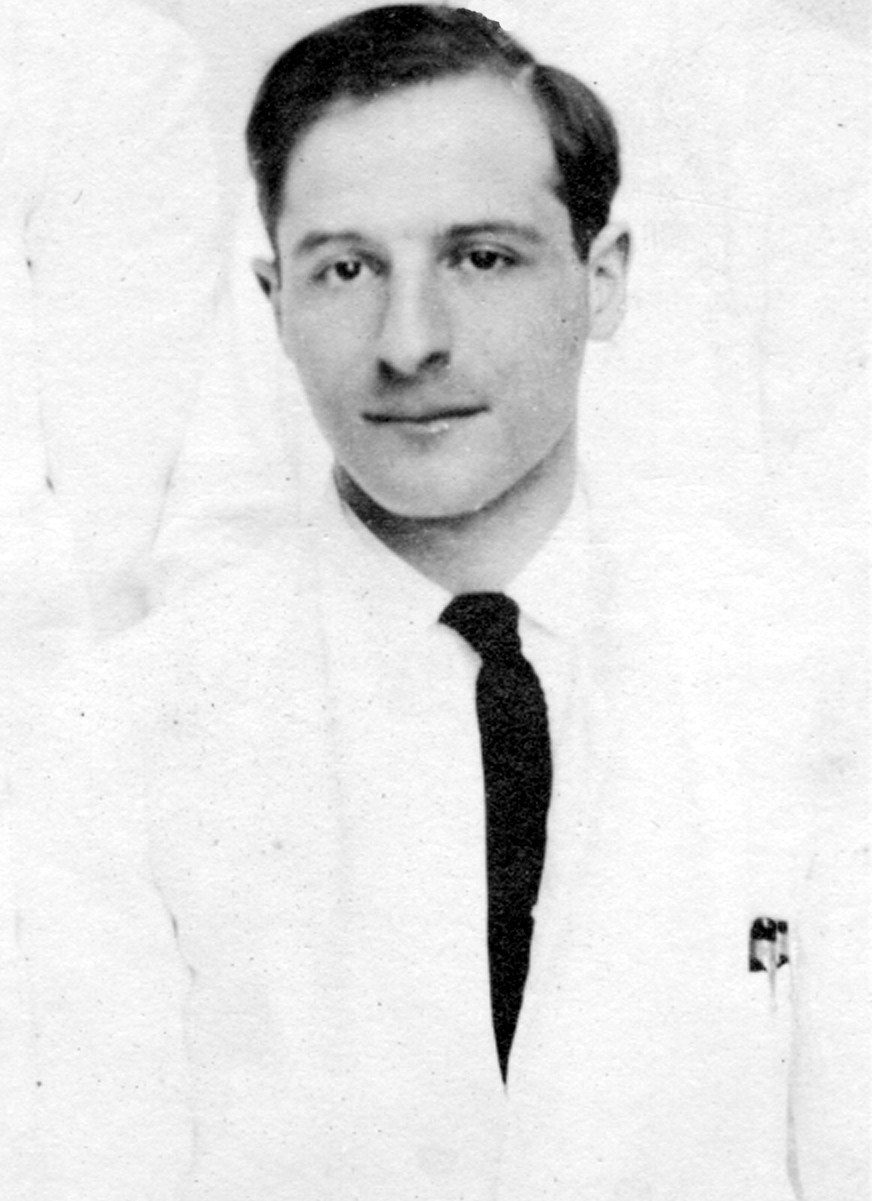
Harry Plotz, MD as a Mount Sinai intern in 1915
Since this was such an important public health problem, in 1915, Mount Sinai’s Trustees took the unusual step of agreeing to fund a trip to gather blood specimens in the Balkans, where there was a typhus outbreak – and the early stages of World War I. As noted in Wikipedia: “disease ravaged the armies of the Eastern Front, where over 150,000 died in Serbia alone. Fatalities were generally between 10% and 40% of those infected and the disease was a major cause of death for those nursing the sick.”
The research results of this trip were described by the physicians Harry Plotz and George Baehr in a 1917 paper in the Journal of Infectious Diseases. The details of the trip itself are described in the 1916 Annual Report of The Mount Sinai Hospital This narrative also describes an additional trip by Dr. Peter Olitzky to Mexico, also funded by Mount Sinai, when the researchers in Europe were taken prisoner by the Austro-Hungarian government. This lengthy quote provides the Trustee President of Mount Sinai’s description of the events of 1915-16:
In pursuance of my remarks of last year in regard to the typhus expedition to Serbia, I wish to state that Drs. George Baehr and Harry Plotz after many difficulties established a laboratory at Belgrade in a hospital directed by the American Red Cross. Thirty-six hours before the bombardment of Belgrade, they left for Uskub and there set up a laboratory in the Lady Paget Hospital, and shortly thereafter the town was occupied by the Bulgarians. Very soon afterwards they were invited by the Bulgarian and Austrian Governments to work under their auspices. They then left for Sofia and afterwards went to Vienna, Lemberg and into Russia….
Because of the fact that Drs. Baehr and Plotz during the first six months of their stay in Europe, practically did not come in contact with typhus fever, it was considered important to send a second expedition into Mexico to determine the cause of the Mexican typhus fever, and to carry on other work which at that time we were not sure could be carried on in Europe. The second expedition consisted of Drs. Peter K. Olitzky and Bernard S. Denzer, accompanied by Mr. Irving Brout, a laboratory helper, and the expedition was under the guidance and care of Dr. Carlos E. Husk, a prominent surgeon attached to the staff of the American Smelting & Refining Co. The expenses of the expedition were defrayed in part by Trustees of the Mount Sinai Hospital and in part by the American Smelting & Refining Co.
It was first decided to go to Aguascalientes, but after the expedition reached Matehuala it was determined to remain there, as even at that distance from the border the danger, because of dis- turbances of international conditions, was very great. Early in March, because of the increasing danger in which the men were placed, they were requested to return. The members of the expedition did not, however, leave, because Dr. Olitzky had been stricken with a severe attack of typhus fever. Very shortly thereafter, the plants of the American Smelting & Refining Co. throughout Mexico were closed down, and Dr. Olitzky had to be removed to Laredo, Texas. Just before the departure Dr. Husk, who had been of the greatest aid in the accomplishment of a remarkable piece of work within four weeks, also fell ill of typhus fever, and was brought into Laredo in a very serious condition. Dr. Olitzky after going through a most dangerous attack of the disease, recovered, but unfortunately it proved impossible to save Dr. Husk’s life.
During the course of this expedition the same germ was found in the typhus fever cases in Mexico as had been found in New York and as was found by the members of the European expedition in Serbia, Bulgaria, Austria and Russia. Apart from that, the typhus germ was cultivated repeatedly from lice, which have in recent years been considered the agent in transferring typhus fever from one person to another. Some further scientific studies were made, and vaccination done on a rather large scale. The results of the vaccination cannot be determined at the present time because of the unsettled conditions in Mexico.
In the end, no successful vaccine has been developed for typhus, but antibiotics and public health measures have made it a treatable, rarely fatal disease in the U.S.
The story of typhus and Mount Sinai is important because it shows the institution’s commitment to research and developing new treatments during times of crisis. As shown here, this commitment is not solely from the medical and scientific staff, but also from the Trustees and supporters of Mount Sinai. When times are dire, as in today’s COVID-19 pandemic, Sinai finds a way to enable the work to get done to advance medical knowledge and improve the treatment of patients.
May 12, 2020
This year the world marks the 200th anniversary of the birth of Florence Nightingale (1820-1910.) Her name is known around the world and nurses everywhere enjoy the fruits of her labors today. She lived a long time ago in a very different world, but she enunciated the basic philosophy of modern nursing, and introduced statistics into the study of disease.
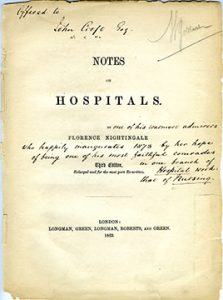
The Aufses Archives has copies of two of Miss Nightingale’s books: Notes on Nursing and Notes on Hospitals. The Mount Sinai Hospital School of Nursing, which existed from 1881-1971, had a small collection of Nightingale letters that they had gathered over the years. Some of these were given to the Columbia University School of Nursing in 1953, as shown in the image below.
From the Aufses Archives

Hospitals, schools of nursing, archives, and history of medicine collections will be marking the 200th anniversary of Florence Nightingale this year with celebrations, blog posts, exhibits and lectures. Here are links to just a few of those celebrations going on this year:
Nightingale: Lady and Legend at the National Library of Medicine: https://circulatingnow.nlm.nih.gov/2020/05/12/nightingale-lady-and-legend/ This includes this note on sources: The National Library of Medicine’s holdings of Nightingale materials are (unsurprisingly) extensive, with over seventy printed titles and editions. In addition, the Library holds a group of Nightingale letters written between 1845 and 1878, all of which may be read as part of the Florence Nightingale Digitization Project, and a copy of an oral history interview conducted by M. Adelaide Nutting (herself a giant in the history of nursing) in 1890. A transcript is available at http://oculus.nlm.nih.gov/2935116r.
A blog post on the University of Maryland, Baltimore School of Nursing ties to Nightingale: https://www2.hshsl.umaryland.edu/hslupdates/?p=4177
A blog post at the UCLA Library about the Elmer Belt FN Collection and other Nightingaleiana we have and use: https://www.library.ucla.edu/blog/special/2020/05/11/happy-birthday-florence-nightingale
Finally, there is a special exhibit at the Florence Nightingale Museum in London called Nightingale in 200 Objects, People & Places https://www.florence-nightingale.co.uk/200objects/ Sadly, the Museum is closed due to the pandemic and is struggling financially. As they note:
Nursing, washing your hands and evidence based-healthcare, pioneered by Florence Nightingale, have become more important than ever before and we’re calling upon our friends and supporters to help us preserve her story and legacy.
Apr 10, 2020
This is a guest blog post by Colleen Stapleton. Colleen is a Patient Navigator with the Liver Education and Action Program (LEAP) at Mount Sinai, where she works to improve linkage to care for patients living with Hepatitis C. Colleen is an advocate for innovative health literacy strategies and a volunteer with the the Arthur H. Aufses, Jr., MD Archives at the Icahn School of Medicine at Mount Sinai, where she hopes to complete a history project mapping women’s contributions to the hospital.
Inspiration
Every Tuesday and Thursday before the global shutdown due to SARS-CoV-2, I left my office on the Upper East Side of Manhattan and walked a few blocks down to the Icahn School of Medicine at Mount Sinai, the Annenberg Building on 5th Ave. The building, part of Mount Sinai Health System’s main hospital complex, is a labyrinth of offices and meeting spaces. On the 10th floor, next to IT offices and tucked behind the Otolaryngology suite, is the office of the Arthur H. Aufses, Jr., MD Archives.
I started volunteering with the archives as a way to keep in touch with my personal interests while working as a patient navigator on a public health project in the Mount Sinai Hospital Liver department. My interest in medical devices, most notably the Dalkon Shield IUD tragedy, had introduced me to historian Susan Perry’s fantastic project that took shape in her 1985 book Nightmare.
Perry’s work inspired me to scheme: how could I sharpen my historical eye? How could I hone my training in visual history and explore my personal investment in the stories of women in medicine? What I found in my project scanning and cataloguing Mount Sinai Health System newsletters, however, was much more upbeat than the project that had originally inspired me.
When I reached out to Mount Sinai’s archive I was generously invited to join a team dedicated to preserving the accomplishments of Mount Sinai providers, scientists, and workers. My lunch-hour task would be to make the Archives’ collection of newsletters more accessible to our archivists, and if possible the Archives’ online readership.
Collection

The first issue of The Mount Sinai Hospital News, which ran from 1958-1982
The Aufses Archives has many collections of newsletters. I am starting with the “Mount Sinai Hospital News.” The series consists of several large folders containing two sets of the title. The first newsletter set, set “one”, is known as the “preservation set.” As such, it isn’t handled frequently and contains the best copies. Set “two” contains the copies of the newsletter that are meant to be handled. This handling may occur when inquiries come in from several sources, including relatives of nursing school alumnae, providers previously employed by the hospital or medical school, and hospital or school departments sourcing historical projects, among others. Both sets are stored among the other contents preserved by the Archives.
The archives are not a museum, and so they contain mostly paper-based items and files pertaining to the history of the hospital and medical school. In addition to the collection of newsletters, the Archives includes photographs, meeting minutes, office files, and miscellanea. The collection does house selected objects, including some medical devices, dolls, and even a moulage kit from the 1990s recently passed along to the Emergency Department for use in emergency drills. One of the oldest objects, a ledger indicating notes from one of the first Mount Sinai Beth Israel board meetings, is written by hand in Yiddish and dates back to the 1890s.
The Plan
At the start of the project, the team discussed plans for indexing a collection of newsletters. Would we keep an Excel file of key terms, titles, and dates? Could we also digitize the newsletters? After thinking about the “what” that we would like to make available, we discussed the “how” and “why” of the project. How would the Archives’ online readership access tools to search the newsletter collection? Would we be able to leverage resources to make every issue available online? What were the costs and benefits of spending time uploading each issue digitally?
I was happy to volunteer my help with scanning the newsletters, due in part to my history with an old archive project at the Everson Museum of Art in Syracuse, NY. As a curatorial intern I had been dying to scan the museum’s collection of newspaper clippings highlighting exhibitions and visits by Yoko Ono and John Lennon among other fascinating historical happenings! As it happened, our crew in Syracuse was limited by resource shortages, and scanning would have to be pushed to the next summer.
After some thought and research into searchable PDF text formats, my inclination to scan and upload every issue into our database (then online) was accepted! I was carefully handed a small pile of newsletters, then headed into our neighboring IT office to commandeer the scanner for an hour. The process of scanning had begun!
Watch for Part II, coming soon.
Jun 21, 2018
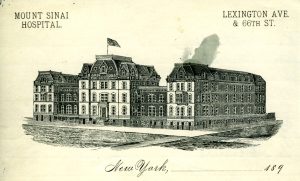
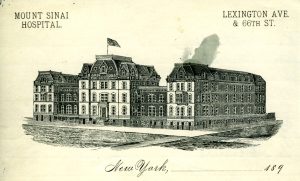
The second site of the Hospital on Lexington Avenue
This is an excerpt from the minutes of the Board of Directors of The Mount Sinai Hospital, March 11, 1888. It is a report from Mr. De Witt J. Seligman, a Director, concerning the proper verification of deaths occurring in the Hospital. The punctuation has not been changed. It provides an interesting view into what was then – and now – a very important issue: how to determine when someone is, in fact, dead.
“Mr. Seligman who was appointed a committee of one…read the following report:
To the Board of Directors of Mount Sinai Hospital:
Having been appointed at the last regular meeting of your Board a Committee of one to look into the matter of certifying to deaths I beg to submit the following report.
In getting at the facts of this matter I have seen three doctors of our visiting staff, the Pathologist of the New York Hospital, the House Surgeon and the House Physician of Mount Sinai Hospital and the Superintendent of Mount Sinai Hospital. There can be no doubt that it happens at times that patients are declared dead before life has become extinct. The Superintendent of our Hospital informs me that on one occasion a nurse told him that her patient was dead and that she was going to announce it to the doctor. The superintendent, Mr. Hadel, went to the Ward and found the alleged dead man sitting bolt upright.
A man informed our Superintendent, Mr. Hadel, that when he was a patient at Blackwell’s Island he was being carried from the Ward to the dead house. On the way they passed through the open air and the effect was that the man on the stretcher became revived and lived to tell this tale of carelessness to our Superintendent. Only this winter a relative by marriage of my wife was, I am informed, declared dead by a physician, but today that same man is as lively as a cricket. Had he been a patient of the Mount Sinai Hospital might he not under our present rules, have ·been hurried from his warm bed in the Ward into the death house and there frozen to death in a short time?
The Pathologist of the New York Hospital informs me that the Ambulance surgeon of the New York Hospital has been repeatedly in doubt as to whether a patient was dead or not and the same Pathologist of the New York Hospital tells me that a certain Dr. Ridlow thought a patient was dead and but two hours later the patient showed life; on the following day Dr. Ridlow again thought that the same patient was dead but even after that on the second day the patient showed life. There was in this case trouble with the heart. An intelligent gentleman connected with the Mount Sinai Hospital as a Director informs me that he and his wife have a mutual agreement by which in the case of the supposed death of one of them, the survivor is to carry out the following agreement: the word of the family physician is not to be taken that death has come but an outside physician is to be summoned to apply the death tests. After that is done no ice is to be placed on the body for 8 hours and the burial is not to take place for three days. In a large institution like ours where deaths are naturally occurring continually, the question arises, what method shall we adopt to avoid the possible mistake of hurrying a supposed corpse into the dead house where in case some life is still in the body it would soon by the sudden change of temperature be frozen out of the body.
One of our visiting physicians whom I saw suggested that the supposed corpse be placed in a warm room for 6 hours and that after 6 hours a second examination be made and then if no sign of life be found place the corps in the dead house. If decomposition has already set in this 6 hours additional precaution, the said visiting physician thought, ought not be taken, nor ought it be taken in warm weather when the cool temperature of the dead house would even aid to revive the flickering flame of life.
This idea seems to me the best idea that was suggested provided it be conscientiously carried out at the Hospital. But whatever rule you may make, one thing is sure and that is that no one but the House Physician on his side and no one but the House Surgeon on his side ought to make the death tests and in each and every case the House Physician or the House Surgeon ought to feel and bear the whole responsibility. To this end I would recommend that we have printed slips which shall run about as follows:
Mount Sinai Hospital, N. Y.
This is to certify that I have this day carefully examined __________________________
a patient of Mount Sinai Hospital in Ward No.____ Bed No.____ and found (him or her) dead.
These slips are to be signed only by the House Surgeon on his side of the Hospital and all these slips are to be kept by the Superintendent of Mount Sinai Hospital in a book for that purpose. In consultations with Drs. Rich and Walsh, the House Surgeon and House Physician of this Hospital, I find that there are no rules as to who shall declare that life has left a patient. Dr. Rich informed me that he always attended to this but Dr. Walsh informed me that in nearly all cases he did and in the remaining cases he left the investigation of the alleged corpse to any doctor, it mattered not which one.
The Pathologist of the New York Hospital informs me that at the New York Hospital the House Physician or the House Surgeon and nobody else testifies to death and even if he has been but a short time previous to death say three times at the bedside said House Physician or House Surgeon is personally compelled to go to the Ward and examine the patient after he has been declared dead. Even at night at the New York Hospital the House Physician or the House Surgeon is compelled to go to the body and examine it.
It may be of interest to you to know that at the New York Hospital every single corpse is washed and put in a shroud and as this operation usually takes half an hour or more, in the opinion of the Pathologist of the New York Hospital who gave me this information, is an additional safeguard against treating the patient as dead before life has left the body.
A great deal more could be written on this important subject, but I think I have written enough to make it clear that this Hospital should have the most stringent rules that can possibly be made in the matter of death certification.
Respectfully submitted
(signed) DeWitt J. Seligman
Mr. [Isaac] Wallach moved that the report of Mr. Seligman dated March 11, 1888 be spread on the minutes in full and that the recommendations contained in said report that the House Physician and House Surgeon must examine persons supposed to have died and sign certificates of death and no one else, in the manner suggested in said report.
That a book be provided for the purpose by the Comm. on Printing.
That the suggestion to place alleged dead persons for 6 hours in a warm room from and during cold months before such bodies are placed in the dead house be referred to the Executive Committee to provide the room if possible.
These provisions are intended as safeguards to prevent the slightest possibility of patients being placed in Dead House who may be apparently dead but not actually so. This whole motion of Mr. Wallach was adopted.
May 18, 2018
By some remarkable coincidence, many Mount Sinai Health System buildings have been dedicated or opened in May.
The Beth Israel Hospital opened its first facility in a rented loft in May 1890 and then moved to 196 Broadway the next year. In May of 1892 they moved again, this time to 206 E. Broadway and 195 Division St. Beth Israel remained at this location until the completion of the Jefferson & Cherry Street building in 1902. Beth Israel did not have another May opening until May 15, 1966 when the Linsky Pavilion opened.
Beth Israel’s Jefferson and Cherry Street location

The Linsky Pavilion, which opened in May 1966
On May 17, 1855, a religious service was held to inaugurate the opening of The Jews’ Hospital in the City of New York, which became The Mount Sinai Hospital in 1866. Presiding at the inauguration was Rabbi J.J. Lyons, with Rabbis Leo, Sternberger, Rubin, Cohen, Waterman, Schickler and Tebrich serving as cantors.
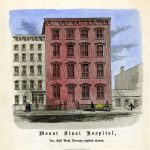
The original building of The Mount Sinai Hospital

The second site of the Hospital
When Mount Sinai had outgrown this site, the Trustees decided to move uptown to the block of Lexington Avenue between 66th and 67th Streets. The cornerstone for the new hospital was laid on May 25, 1870 and the completed hospital was opened on May 29, 1872.

The 1904 building along 100th Street
Within 25 years, the Hospital had again filled its site and decided to move to its current home next to Central Park, between 100th and 101st Streets. The Park ensured that the hospital would not again get surrounded by the bustle of the City’s streets. The cornerstone for this new hospital was laid on May 22, 1901. In May 1922, Mount Sinai marked the completion of a massive expansion project that extended the hospital across 100th Street down to 99th Street. This included 1184 5th Avenue, which today is the oldest building on the Mount Sinai campus.
On May 23, 1952, The Mount Sinai Hospital celebrated the dedication of the Klingenstein Pavilion on 5th Avenue.
This was built as Mount Sinai’s Maternity Pavilion, and remains the home of our OB-GYN department. At the same event, the Atran Laboratory and the Henry W. Berg, MD Laboratory buildings were both dedicated as well.

The Klingenstein Pavilion on 5th Avenue

Vice President Ford and Walter Annenberg looking at the portrait of Mrs. Annenberg at the dedication in 1974
And finally, in perhaps Mount Sinai’s biggest dedication, on May 26, 1974, the new Mount Sinai School of Medicine welcomed Vice President Gerald Ford and the Annenberg family to celebrate the formal dedication of the Annenberg Building. When this building opened, it was the thought to be the largest space in this country devoted to medical education.

St. Luke’s Hospital on 5th Avenue
The Mount Sinai Hospital was not alone in its fascination with May for buildings. On May 21, 1857, the St. Luke’s Hospital chapel opened at the Hospital’s first site and a year later (May 13, 1858) the hospital itself opened at 5th Ave between 54th and 55th Streets.
The Woman’s Hospital in the State of New York, which became the Women’s Division of St. Luke’s Hospital in 1952, also had a May dedication tradition. On May 4, 1855 the Woman’s Hospital was opened at 83 Madison Avenue. Almost 50 years later, on May 17, 1904, the cornerstone was laid at a new site at Amsterdam Avenue and 110th Street.

The first home of the Woman’s Hospital

The 1904 west side Woman’s Hospital building
Finally, on May 25, 1965 the Woman’s Hospital opened in a separate building on the St. Luke’s campus on Amsterdam Avenue and 114th Street.