Jan 10, 2022
In a previous blog post, we looked at Beth Israel Hospital’s role in the 1918 Influenza Epidemic. Since then, we’ve done further research into the World War I correspondence in the Beth Israel records, as well as the Beth Israel Board of Directors and Committee minutes, which both provided rich details to supplement this history.
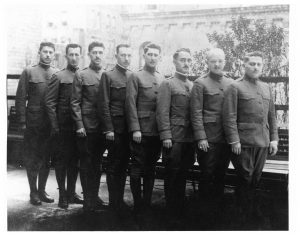
In early March 1918, influenza had reached New York. By March 25, 1918, an unknown correspondent (likely Louis J. Frank, Beth Israel Hospital superintendent) wrote that there was “quite an epidemic in the City of Grippe,” referring to New York City as literally the “City of the Flu”. As World War I continued on, many Beth Israel workers had joined the war effort, and their correspondence with the hospital describes the epidemic on the front lines. The first wave of the flu was relatively mild, and on May 13, 1918, Dr. Alfred A. Schwartz of the American Expeditionary Force, reported as much from France:
“I have been appointed Otolaryngologist to the contagious disease wards at the camp hospital and altho [sic] the title sounds like work, there must first be complications to the infectious diseases, and secondly…there must be some patients to have the diseases, and fortunately there is little to do.”
As the second, more deadly wave swept the world, the topic of influenza became more pressing in the correspondence, and was increasingly addressed in the Board minutes. In the November 17, 1918, minutes, the Board noted that back on the home front in New York, Beth Israel attended to “50 to 60 cases of Influenza a day during the height of the epidemic and…our records of cures was high, and our record of deaths was very low.” This is a significant deviation from the previous blog post, which stated that only twenty-nine patients total were treated during the epidemic at Beth Israel. Sources conflict on this point.
Staffing was amongst the most pressing issues at this time – with much of the medical staff overseas, Louis J. Frank, himself recovering from the flu, commented in a letter from October 23, 1918: “Our whole force is gone. If you were to come back today, you wouldn’t find a familiar face…From a house staff of 15 we have been reduced to a staff of five, and of the five, three have been laid up on account of influenza.” He goes on to describe the issue of hiring enough nurses, which was making him “frantic.” Superintendent Frank was a proponent of the conscription of women, “especially those women who have the vote,” to counteract staffing shortages in nursing in the war and at home.
The Board of Directors’ minutes reflect similar staffing concerns. The minutes for November 17, 1918, stated: “During the epidemic the Surgical Staff consisted of one man, the others became infected with the disease. On the Medical side we only had two men, the others also sick.” This appears to have resulted in redeployment of other clinical workers, and the Board resolved on “the discontinuance of the work of the Polio Department on account of the epidemic of Influenza and Pneumonia to release the doctors and nurses connected with the clinic for the more important work.” The minutes also noted that the “pupil nurses” from Beth Israel Training School for Nurses (today’s Phillips School of Nursing at MSBI) “after their day’s work was over, did extra work in the district on these cases, spending an hour or two on emergency cases requiring special care.”
The close of 1918 marked a turning point. With the War over, and a dwindling number of cases following the peak of the second wave, the end was in sight. In a letter from November 27, 1918, Superintendent Frank wrote:
“Things are getting into shape at the Hospital. We were considerably upset on account of the War, shortage of help, doctors, nurses, the Influenza epidemic, and the general anxiety, but with victory came a relaxation and we are now awaiting the homecoming of you men who have done so much to achieve this victory.”
The Board also noted, grimly, on November 17, 1918, that Beth Israel was “the only Hospital [in New York City] that didn’t lose a nurse, a doctor, or an employee by death.” On January 19, 1919, the Board moved to give House Staff and pupil nurses bonuses for their contributions and made especial note of the nurses’ service: “pupil nurses…after their trying [work and school] day of 12 and many times 14 hours, went out in the tenement houses and did extra work for several hours. Of course, this work was not for patients of the Hospital, but it was nevertheless our work, for they were the poor sick of our neighborhood.”
On November 23, 1919, the Board made note of the U.S. Public Health Service’s prediction that the influenza epidemic would return. Fortunately, this never came to pass. By 1920, the virus mutated to cause only ordinary cases of the seasonal flu, and the epidemic was effectively over.
Sources:
More resources on Mount Sinai Health System Hospitals and World War I are available here.
Authored by Stefana Breitwieser, Digital Archivist
Nov 10, 2021
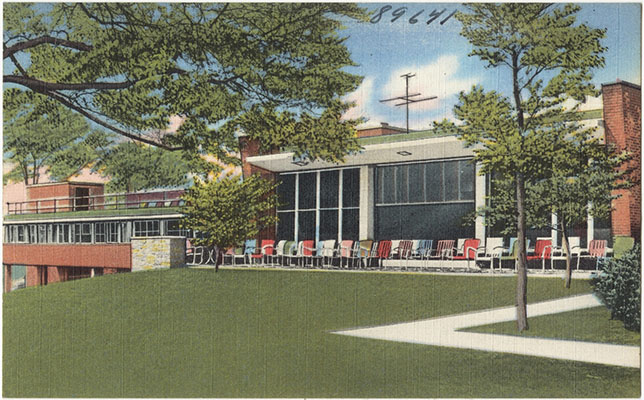
The Neustadter Home was created by a provision in the 1905 will of Caroline Neustadter to serve as a convalescent center for women patients after leaving the hospital. It opened in July 1919 on the northeast corner of Central Park Avenue and McLean Avenue in Yonkers, on land once owned by Boss Tweed, leader of Tammany Hall. In 1936, an agreement was reached between The Mount Sinai Hospital and the Neustadter Home whereby Mount Sinai could send patients to the facility. Three years later, men began to be admitted as well.

The original Neustadter Home in the 1950s
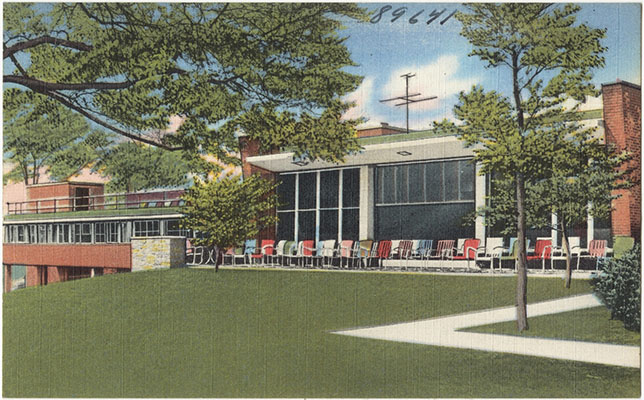
The Moses Weinman wing, opened in 1949
As hospitals saw the increasing value in freeing up beds for more acute cases by discharging patients to rehabilitation hospitals, Neustadter needed to expand. The Moses Weinman wing was added in 1949, bringing the institution up to 69 beds from the previous 56. The facility also enhanced its medical care services. To reflect this evolution, the name was changed from the Neustadter Home to the Neustadter Convalescent Center in 1954. Over the years, the patient population was composed primarily of post-surgical cases. As the 1971 Mount Sinai Annual Report on convalescent care said: “So often before we have described the true function of Neustadter as a bridge that spans illness to complete recovery.” In 1969, Mount Sinai was given preferential use of the Center and eventually the Neustadter Board members and the medical staff were affiliated with Mount Sinai.
The Convalescent Center did not have a bright future, however. In a 1959 study of Neustadter, only 24% of patients could afford the full weekly charge of $84. Money was a perennial problem. Also, because the Home was twelve miles from Mount Sinai Hospital, it was hard to provide follow-up care by physicians. In 1972, the Neustadter Board dissolved and transferred their assets to The Mount Sinai Hospital. The next year, Mount Sinai sought to sell the Convalescent Center. The sale for $1 million to a local Hebrew high school was announced in 1973, but the school struggled to make the payments. The matter sputtered along for a few years, and in 1980 the property was finally sold to a realty company. In 1983, a shopping center opened on the site, including a large Waldbaum’s grocery store. The shops remain; the Waldbaum’s is gone. The Neustadter Convalescent Center has also totally disappeared.
For information on what archival material the Aufses Archives has relating to the Neustadter Convalescent Center, click here.
Aug 18, 2021
The Upper East Side home of The Mount Sinai Hospital and the Icahn School of Medicine at Mount Sinai spans continuously from 101st St down to 98th Street, with other buildings arrayed nearby. To achieve this continuous campus, what had once been 99th and 100th Streets between Madison and Fifth Avenues have disappeared. How and when did that happen?

View along 100th St., around 1937
The Mount Sinai Hospital moved to 100th Street in 1904, taking up the whole block between the avenues and up to 101st Street. In 1911, the Hospital started buying lots on the south side of 100th Street in anticipation of a large expansion program. By 1921, those new buildings stretched from Fifth Avenue across but not quite to the end of 100th Street. The street was used for physician parking, and in December 1949, New York City deeded the bed of 100th Street to Mount Sinai. It continued as parking for a few more decades, but with the construction of the Guggenheim Pavilion starting in 1986, the street disappeared into a plaza between the original buildings and the new.
The story on 99th Street is very similar: Mount Sinai had expanded to having buildings spread along the northern side of the block. At the end of the 1950s, when construction of the Klingenstein Clinical Center (KCC), fronting onto the corner of Madison and 99th Street, was being planned, Mount Sinai sought the help of the City, and in August 1958, the road bed of 99th Street was deeded to Mount Sinai.
And what about the former streets? Once the construction on KCC was finished, this area became known as the Hospital Gardens, and graduation ceremonies for our School of Nursing, as well as special events were held out there. The plaza across 100th Street was covered in bricks, and a large sculpture called La Sfera Grande by Arnaldo Pomodoro was placed there in 1974. In the late 1960s, all of the buildings along the former southern side of 100th Street and the northern side of 99th Street were torn down to make way for the Annenberg Building. The Gardens became Ross Park, and today the Sfera Grande sits adjacent to the Nathan Cummings Atrium in the Guggenheim Pavilion. This is only appropriate since Mr. Cummings had originally given Mount Sinai the sculpture.

Nursing School graduation in the ‘Gardens’ in 1961. Note that KCC is being built in the back left of the image.
Aug 3, 2021
On August 27th, it will be 165 years since the first baby was born at The Mount Sinai Hospital in 1856. The mother was a Mrs. Lichtenstein. She named the baby Isaac Touro, in honor of a Hospital benefactor, Judah Touro (1775-1854), who had helped support the young Jews’ Hospital in New York, as Mount Sinai was then known. (Judah Touro also gave money for the founding of Touro Infirmary in New Orleans and today’s Touro College and University System is named for Judah and his father Isaac.)
Isaac Touro Lichtenstein was one of two babies born in the Hospital during its first year of operation. Until the 1920s, most babies were born at home or in one of the specialized women and child care hospitals around the City. This meant that many general hospitals, including Mount Sinai, never felt the need to add a formal obstetrical service to their offerings, thus limiting the number of babies born at the hospital over the years.
By the 1920s, as hospital births began to rise around the country, the Mount Sinai medical staff started to talk to the Board of Trustees about adding obstetrics. As the doctors saw it, the problems arising from not having babies born at the Hospital were: the Gynecology staff could not admit their obstetrical patients to Mount Sinai; there was no obstetrical training for the GYN residents, nor was there training for the pediatrics residents in newborn care. The last also applied to The Mount Sinai Hospital School of Nursing, which affiliated with the Sloane Hospital for Women so students could fill the gap in their education.
While the Trustees were increasingly sympathetic with the request to add an obstetrical service, it wasn’t until the middle of the 1940s that concrete plans were made for the erection of a new building to house obstetrics and gynecology, today’s Klingenstein Pavilion on Fifth Avenue. Every new building demands a fundraising campaign to make it a reality. Mount Sinai had just finished a major expansion that ended in 1922, with the addition of a new School of Nursing building and a semi-private pavilion seen as the next priorities. When these two buildings opened, the Depression was in full swing, which sapped Hospital and potential donor resources. This was followed quickly by World War II, but by the mid-1940s, the Hospital could see a window of opportunity on the horizon.
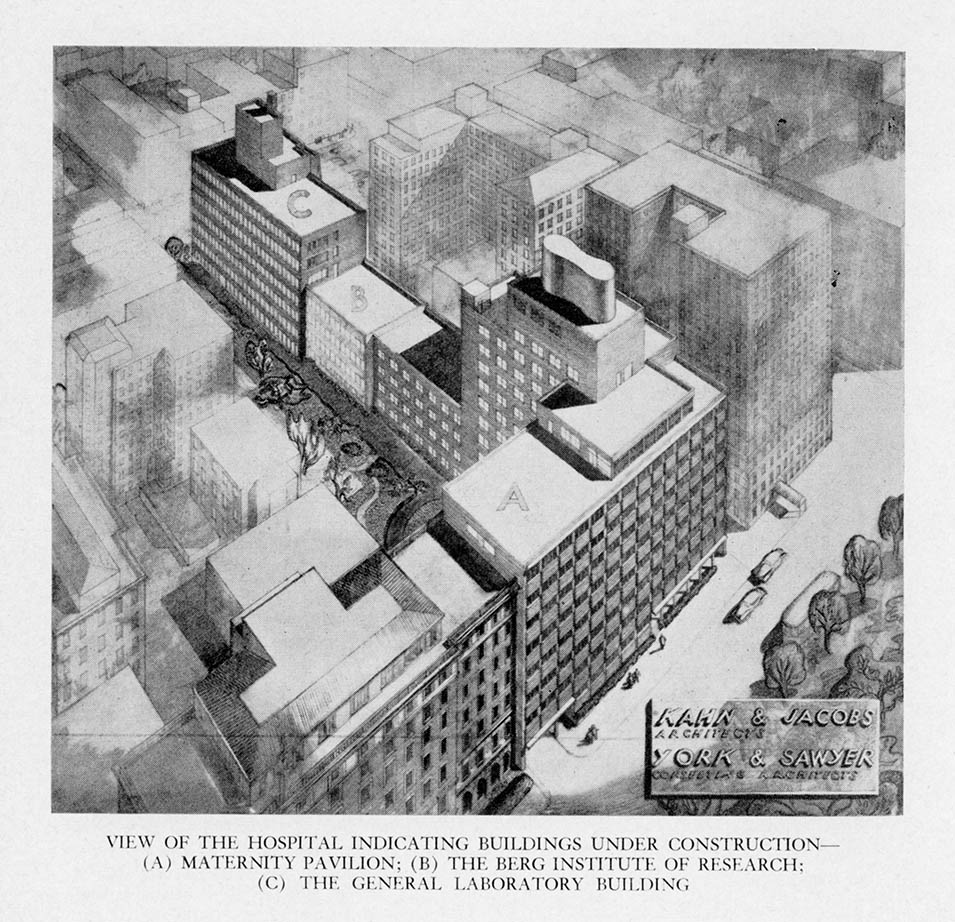
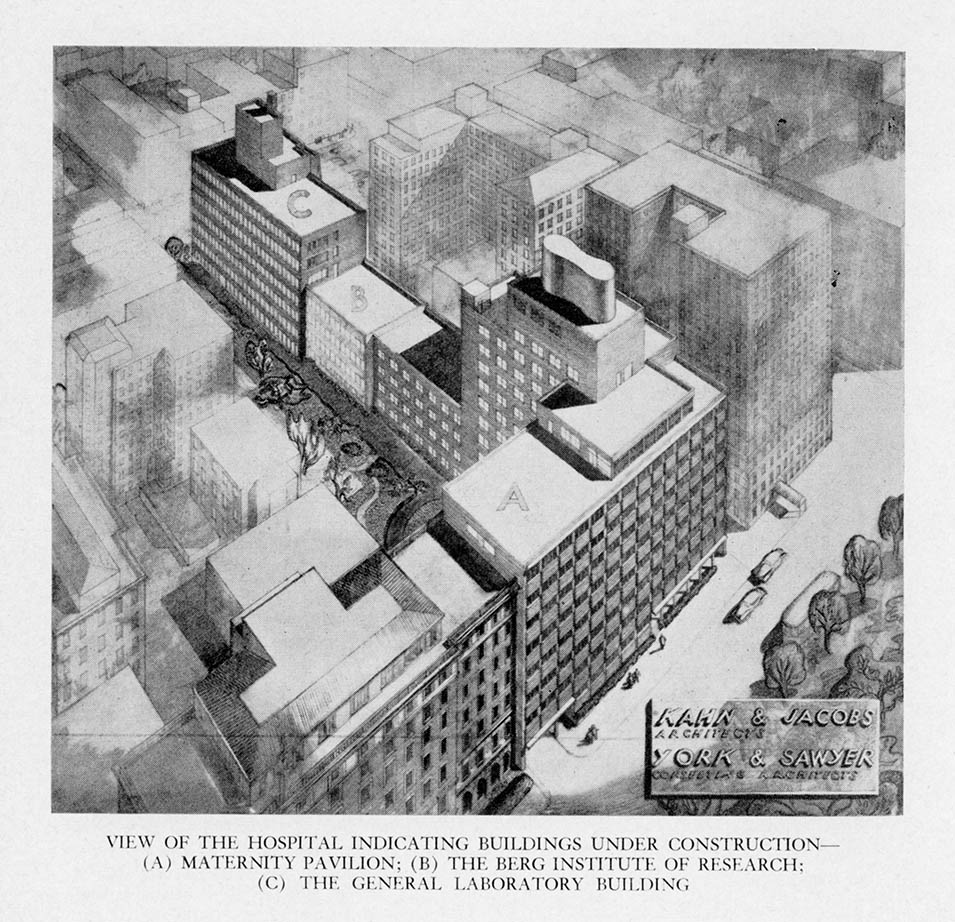
A fundraising campaign was begun when the war ended and on July 22, 1948, ground was broken for three buildings: the Klingenstein Pavilion, and the Atran and Berg Laboratories. In 1952, the obstetrical service started to operate as the building slowly opened. July marked the start of Mount Sinai’s first Prenatal Clinic, and the first prenatal clinic for women with diabetes in New York City started in the fall. The first OB patients were admitted in October, with the first baby born October 29, 1952 – 96 years after Isaac Touro Lichtenstein.
Jun 21, 2021
I recently spent some time reviewing the President’s Report section of the Annual Report of The Mount Sinai Hospital from 1921 (linked here, starting on page 190). The President then was George Blumenthal, a devoted trustee, and a smart businessman who had recently guided the Hospital through a major expansion program, the uncertainties of World War I, and the influenza epidemic of 1918. Reading the report reminded me of the joys – and problems – with reading primary historical sources: it is very easy in hindsight to see connections between two times that may not be related, and simple observations can seem very prescient.
Don’t get me wrong, parts of the report are very dated and irrelevant to today: the Hospital was unable to afford radium to use in patient treatment, and so that service was not provided. There was also a section on issues related to fund raising through the Federation of Jewish Charities (today’s UJA-Federation). But still, there were many issues that would seem familiar to our current leaders. The Hospital was perennially short of money, but after the epidemic and the war, wages were rising quickly for what today would be called “essential workers”. Adding to this was a restrictive immigration policy that limited the labor pool. The inability to hire as many trained nurses as they needed was a continuing struggle as well, something the whole country recognizes today.
George Blumenthal, President of The Mount Sinai Hospital from 1911-1938
And yet Blumenthal made the case – as we do today – for why private hospitals like Mount Sinai deserve the philanthropic support of the people. He says:
It is absolutely essential that private institutions like Mount Sinai should be leaders of progress in hospital work…. To discover, test and demonstrate new methods of treatment is recognized as one of the functions of private institutions and it is one of the strongest reasons for their existence and constitutes their most important claim on the generosity of the public which supports them.
A couple of pages later, Blumenthal makes a bold statement about the importance of Mount Sinai being a teaching hospital. At this time it had loose clinical ties to both Columbia and NYU. He envisioned something more:
A Hospital possessing the clinical and laboratory resources of Mount Sinai should have university affiliation or if this be impracticable should independently utilize its organization for teaching purposes, for in no other way can the fullest benefits be derived from the intensive study of interesting, varied and often perplexing clinical material. We hope the day is not very far off when work on these lines can be done either through affiliation with one of the many teaching institutions located in our city or by independent action.
And “independent action” it was. Even with academic affiliations with various medical schools, in the 1950s Mount Sinai was not satisfied that they were living up to their potential in terms of training the next generation of physician/scientists or using their immense clinical material for creating new medical knowledge to advance patient care. In 1963, the Trustees received a charter to create their own medical and graduate schools. The Mount Sinai School of Medicine opened in 1968.