Apr 10, 2020
This is a guest blog post by Colleen Stapleton. Colleen is a Patient Navigator with the Liver Education and Action Program (LEAP) at Mount Sinai, where she works to improve linkage to care for patients living with Hepatitis C. Colleen is an advocate for innovative health literacy strategies and a volunteer with the the Arthur H. Aufses, Jr., MD Archives at the Icahn School of Medicine at Mount Sinai, where she hopes to complete a history project mapping women’s contributions to the hospital.
Inspiration
Every Tuesday and Thursday before the global shutdown due to SARS-CoV-2, I left my office on the Upper East Side of Manhattan and walked a few blocks down to the Icahn School of Medicine at Mount Sinai, the Annenberg Building on 5th Ave. The building, part of Mount Sinai Health System’s main hospital complex, is a labyrinth of offices and meeting spaces. On the 10th floor, next to IT offices and tucked behind the Otolaryngology suite, is the office of the Arthur H. Aufses, Jr., MD Archives.
I started volunteering with the archives as a way to keep in touch with my personal interests while working as a patient navigator on a public health project in the Mount Sinai Hospital Liver department. My interest in medical devices, most notably the Dalkon Shield IUD tragedy, had introduced me to historian Susan Perry’s fantastic project that took shape in her 1985 book Nightmare.
Perry’s work inspired me to scheme: how could I sharpen my historical eye? How could I hone my training in visual history and explore my personal investment in the stories of women in medicine? What I found in my project scanning and cataloguing Mount Sinai Health System newsletters, however, was much more upbeat than the project that had originally inspired me.
When I reached out to Mount Sinai’s archive I was generously invited to join a team dedicated to preserving the accomplishments of Mount Sinai providers, scientists, and workers. My lunch-hour task would be to make the Archives’ collection of newsletters more accessible to our archivists, and if possible the Archives’ online readership.
Collection

The first issue of The Mount Sinai Hospital News, which ran from 1958-1982
The Aufses Archives has many collections of newsletters. I am starting with the “Mount Sinai Hospital News.” The series consists of several large folders containing two sets of the title. The first newsletter set, set “one”, is known as the “preservation set.” As such, it isn’t handled frequently and contains the best copies. Set “two” contains the copies of the newsletter that are meant to be handled. This handling may occur when inquiries come in from several sources, including relatives of nursing school alumnae, providers previously employed by the hospital or medical school, and hospital or school departments sourcing historical projects, among others. Both sets are stored among the other contents preserved by the Archives.
The archives are not a museum, and so they contain mostly paper-based items and files pertaining to the history of the hospital and medical school. In addition to the collection of newsletters, the Archives includes photographs, meeting minutes, office files, and miscellanea. The collection does house selected objects, including some medical devices, dolls, and even a moulage kit from the 1990s recently passed along to the Emergency Department for use in emergency drills. One of the oldest objects, a ledger indicating notes from one of the first Mount Sinai Beth Israel board meetings, is written by hand in Yiddish and dates back to the 1890s.
The Plan
At the start of the project, the team discussed plans for indexing a collection of newsletters. Would we keep an Excel file of key terms, titles, and dates? Could we also digitize the newsletters? After thinking about the “what” that we would like to make available, we discussed the “how” and “why” of the project. How would the Archives’ online readership access tools to search the newsletter collection? Would we be able to leverage resources to make every issue available online? What were the costs and benefits of spending time uploading each issue digitally?
I was happy to volunteer my help with scanning the newsletters, due in part to my history with an old archive project at the Everson Museum of Art in Syracuse, NY. As a curatorial intern I had been dying to scan the museum’s collection of newspaper clippings highlighting exhibitions and visits by Yoko Ono and John Lennon among other fascinating historical happenings! As it happened, our crew in Syracuse was limited by resource shortages, and scanning would have to be pushed to the next summer.
After some thought and research into searchable PDF text formats, my inclination to scan and upload every issue into our database (then online) was accepted! I was carefully handed a small pile of newsletters, then headed into our neighboring IT office to commandeer the scanner for an hour. The process of scanning had begun!
Watch for Part II, coming soon.
Apr 30, 2019
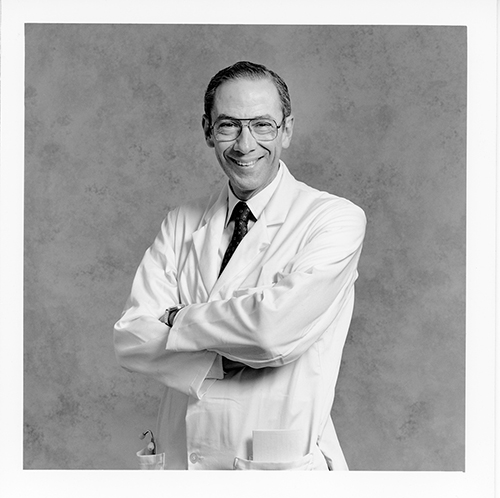
It is with great sadness that we share news of the passing of our dear friend and supporter Arthur H. Aufses, Jr., MD (1926-2019), one of the Mount Sinai Health System’s most respected physicians and Chairman Emeritus of The Ruth J. & Maxwell Hauser and Harriet & Arthur H. Aufses, Jr., MD Department of Surgery at The Mount Sinai Hospital, and Professor in Surgery as well as the Department of Population Health Science and Policy.
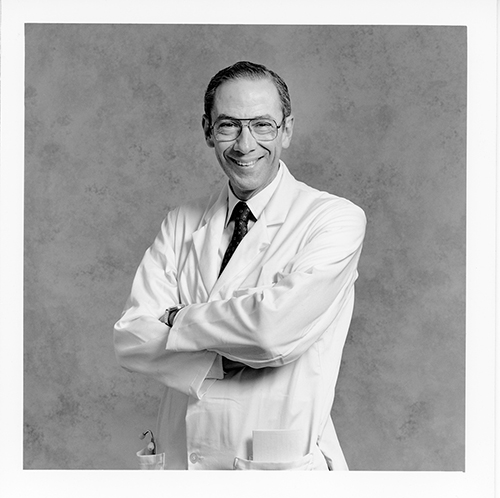
Arthur H. Aufses, Jr., MD, 1926-2019
An innovative leader who served as Chair of the Department of Surgery from 1974-1996, Dr. Aufses ushered in Mount Sinai’s adoption of laparoscopic surgery and oversaw the expansion of ambulatory surgery and the hospital’s transplant program. He organized the surgical team that performed the first liver transplant in New York State in 1988.
Within Mount Sinai, Dr. Aufses served as a mentor to many residents and fellows and helped to break down barriers for women and minority surgeons. Over the years, he received many Excellence in Teaching awards from the Icahn School of Medicine at Mount Sinai, as well as institutional honors, including the Alumni Association’s Jacobi Medallion, and the Alexander Richman Award for Humanism in Medicine. He was the holder of Mount Sinai’s Gold Headed Cane from 1982 to 1997. On 17 occasions, medical students selected Dr. Aufses to administer the Oath of Maimonides or the Oath of Hippocrates at commencement, and on three occasions he was chosen to serve as Commencement Grand Marshal. In May 2003, Dr. Aufses delivered the medical school’s commencement address and was awarded an honorary Doctor of Humane Letters.
In addition to publishing more than 235 research papers and book chapters—many on the topics of surgical education and inflammatory bowel disease—he held leadership roles in many professional organizations. These include the New York Academy of Medicine, the American College of Gastroenterology, the New York Surgical Society, the American College of Surgeons, and the American Surgical Association.
Dr. Aufses also had a keen interest in Mount Sinai’s long and storied history, and published two books on the subject with institutional archivist Barbara Niss. This House of Noble Deeds: The Mount Sinai Hospital, 1852-2002 (New York University Press, 2002), chronicled the 150-year history of The Mount Sinai Hospital, focusing on the accomplishments of the staff since its origin as The Jews’ Hospital in the City of New York. Teaching Tomorrow’s Medicine Today: The Mount Sinai School of Medicine, 1963-2003 (New York University Press, 2005), detailed the first forty years of the Icahn School of Medicine at Mount Sinai.
In April 2017, Dr. Aufses’ support of the Archives was made clear when the Mount Sinai Archives was formally dedicated as the Arthur H. Aufses, Jr. MD Archives.
The staff of the Arthur H. Aufses, Jr., MD Archives will miss Dr. Aufses’ kindness, sense of humor, and selfless service to Mount Sinai. Dr. Aufses was calm and steady in the operating room and in life. He delighted in his trainees’ achievements, and set an example of honesty, integrity, and loyalty for those who followed him. He was a true Mount Sinai Giant.
Jun 21, 2018
The second site of the Hospital on Lexington Avenue
This is an excerpt from the minutes of the Board of Directors of The Mount Sinai Hospital, March 11, 1888. It is a report from Mr. De Witt J. Seligman, a Director, concerning the proper verification of deaths occurring in the Hospital. The punctuation has not been changed. It provides an interesting view into what was then – and now – a very important issue: how to determine when someone is, in fact, dead.
“Mr. Seligman who was appointed a committee of one…read the following report:
To the Board of Directors of Mount Sinai Hospital:
Having been appointed at the last regular meeting of your Board a Committee of one to look into the matter of certifying to deaths I beg to submit the following report.
In getting at the facts of this matter I have seen three doctors of our visiting staff, the Pathologist of the New York Hospital, the House Surgeon and the House Physician of Mount Sinai Hospital and the Superintendent of Mount Sinai Hospital. There can be no doubt that it happens at times that patients are declared dead before life has become extinct. The Superintendent of our Hospital informs me that on one occasion a nurse told him that her patient was dead and that she was going to announce it to the doctor. The superintendent, Mr. Hadel, went to the Ward and found the alleged dead man sitting bolt upright.
A man informed our Superintendent, Mr. Hadel, that when he was a patient at Blackwell’s Island he was being carried from the Ward to the dead house. On the way they passed through the open air and the effect was that the man on the stretcher became revived and lived to tell this tale of carelessness to our Superintendent. Only this winter a relative by marriage of my wife was, I am informed, declared dead by a physician, but today that same man is as lively as a cricket. Had he been a patient of the Mount Sinai Hospital might he not under our present rules, have ·been hurried from his warm bed in the Ward into the death house and there frozen to death in a short time?
The Pathologist of the New York Hospital informs me that the Ambulance surgeon of the New York Hospital has been repeatedly in doubt as to whether a patient was dead or not and the same Pathologist of the New York Hospital tells me that a certain Dr. Ridlow thought a patient was dead and but two hours later the patient showed life; on the following day Dr. Ridlow again thought that the same patient was dead but even after that on the second day the patient showed life. There was in this case trouble with the heart. An intelligent gentleman connected with the Mount Sinai Hospital as a Director informs me that he and his wife have a mutual agreement by which in the case of the supposed death of one of them, the survivor is to carry out the following agreement: the word of the family physician is not to be taken that death has come but an outside physician is to be summoned to apply the death tests. After that is done no ice is to be placed on the body for 8 hours and the burial is not to take place for three days. In a large institution like ours where deaths are naturally occurring continually, the question arises, what method shall we adopt to avoid the possible mistake of hurrying a supposed corpse into the dead house where in case some life is still in the body it would soon by the sudden change of temperature be frozen out of the body.
One of our visiting physicians whom I saw suggested that the supposed corpse be placed in a warm room for 6 hours and that after 6 hours a second examination be made and then if no sign of life be found place the corps in the dead house. If decomposition has already set in this 6 hours additional precaution, the said visiting physician thought, ought not be taken, nor ought it be taken in warm weather when the cool temperature of the dead house would even aid to revive the flickering flame of life.
This idea seems to me the best idea that was suggested provided it be conscientiously carried out at the Hospital. But whatever rule you may make, one thing is sure and that is that no one but the House Physician on his side and no one but the House Surgeon on his side ought to make the death tests and in each and every case the House Physician or the House Surgeon ought to feel and bear the whole responsibility. To this end I would recommend that we have printed slips which shall run about as follows:
Mount Sinai Hospital, N. Y.
This is to certify that I have this day carefully examined __________________________
a patient of Mount Sinai Hospital in Ward No.____ Bed No.____ and found (him or her) dead.
These slips are to be signed only by the House Surgeon on his side of the Hospital and all these slips are to be kept by the Superintendent of Mount Sinai Hospital in a book for that purpose. In consultations with Drs. Rich and Walsh, the House Surgeon and House Physician of this Hospital, I find that there are no rules as to who shall declare that life has left a patient. Dr. Rich informed me that he always attended to this but Dr. Walsh informed me that in nearly all cases he did and in the remaining cases he left the investigation of the alleged corpse to any doctor, it mattered not which one.
The Pathologist of the New York Hospital informs me that at the New York Hospital the House Physician or the House Surgeon and nobody else testifies to death and even if he has been but a short time previous to death say three times at the bedside said House Physician or House Surgeon is personally compelled to go to the Ward and examine the patient after he has been declared dead. Even at night at the New York Hospital the House Physician or the House Surgeon is compelled to go to the body and examine it.
It may be of interest to you to know that at the New York Hospital every single corpse is washed and put in a shroud and as this operation usually takes half an hour or more, in the opinion of the Pathologist of the New York Hospital who gave me this information, is an additional safeguard against treating the patient as dead before life has left the body.
A great deal more could be written on this important subject, but I think I have written enough to make it clear that this Hospital should have the most stringent rules that can possibly be made in the matter of death certification.
Respectfully submitted
(signed) DeWitt J. Seligman
Mr. [Isaac] Wallach moved that the report of Mr. Seligman dated March 11, 1888 be spread on the minutes in full and that the recommendations contained in said report that the House Physician and House Surgeon must examine persons supposed to have died and sign certificates of death and no one else, in the manner suggested in said report.
That a book be provided for the purpose by the Comm. on Printing.
That the suggestion to place alleged dead persons for 6 hours in a warm room from and during cold months before such bodies are placed in the dead house be referred to the Executive Committee to provide the room if possible.
These provisions are intended as safeguards to prevent the slightest possibility of patients being placed in Dead House who may be apparently dead but not actually so. This whole motion of Mr. Wallach was adopted.
May 25, 2018
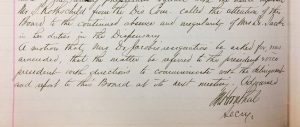
In 1875, The Mount Sinai Hospital selected Mary Putnam Jacobi, MD (1842-1906) to be the Chief of the newly established Children’s Clinic. Abraham Jacobi, MD, her husband, was an important member of the Mount Sinai medical staff and is today considered the Father of Pediatrics in this country. Still, the Trustees did not want him to be in charge of both the inpatient and outpatient services, so Mary Jacobi was appointed. All was well for some years, but in May 1884, the Board of Trustees’ minutes record the “continued absence and irregularity of Mrs. Dr. Jacobi in her duties in the Dispensary.” There was a motion seeking her resignation, but this was amended to instead send the president and vice-president of the Board to speak with “the delinquent” and report back. The subsequent meeting does not have a report on the visit with “Mrs. Dr. Jacobi,” but it is known that she resigned from the staff in October of 1886, more than two years later. Did being “Mrs.” Jacobi save her appointment? Perhaps. The very few other female doctors on staff were known as just Dr. The fact that Mary Putnam was married to Abraham Jacobi probably loomed large in the eyes of the Mount Sinai trustees. He remained associated with the hospital until his death in 1919.
The minutes of the Board of Trustees of The Mount Sinai Hospital, May 1884
Apr 24, 2018
As the spring very slowly arrives, the tired mind often screams for relief from the challenge of processing complex information. So, here is some Mount Sinai trivia that is guaranteed to interest without straining the brain.
Did you know:
…that in the 17th century there were Native Americans living in East Harlem and there was a stream flowing where the Icahn building now stands?
…that the first year The Mount Sinai Hospital was opened (1855-56), we admitted 216 patients, only five of whom were born in the US, and three of them listed their careers as comedians?
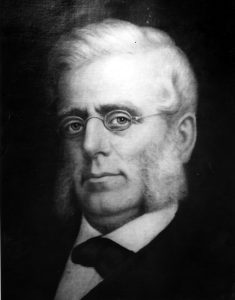
Mount Sinai founder, Benjamin Nathan
…that The Mount Sinai Hospital had a well regarded nursing school that existed from 1881-1971 and that 5 E. 98th Street was the School of Nursing dorm/educational building?
…that when the Hospital moved to its second site at Lexington Ave. and 66th St. in 1872, the Trustees built a large synagogue upstairs and a small operating room in the basement?
…that a Mount Sinai founder, Benjamin Nathan, was murdered in his sleep on a stormy night, and members of his family are still on the Board to this day?
…that Mount Sinai did not have an obstetrical service for the first century of its existence, only offering an OB Service when the Klingenstein Pavilion opened in late 1952?
…that there is a time capsule buried under the directory in the Annenberg Lobby that is scheduled to be opened in 2074, 100 years after it was placed there?
…that Jonas Salk and Henry Heimlich both served their internships at Mount Sinai, Salk graduating in 1942 and Heimlich in 1948?
…that in 1964, Mount Sinai had 1,326 beds, 200 more than we have today?
…that when the first ICU opened at Mount Sinai in 1962, it had five beds and was located in 1184 Fifth Ave., on the 7th floor?
…that in 1993 Mount Sinai School of Medicine became the first in New York State to graduate a class with more women than men?
…that there are at least 43 diseases, syndromes, tests, instruments and phenomena named after Mount Sinai physicians and scientists?